Rate of incidental findings on routine preoperative computed tomography for shoulder arthroplasty
Article information
Abstract
Background
Incidental findings are commonly noted in advanced imaging studies. Few data exist regarding the rate of incidental findings on computed tomography (CT) for preoperative shoulder arthroplasty planning. This study aims to identify the incidence of these findings and the rate at which they warrant further work-up to help guide orthopedic surgeons in counseling patients.
Methods
A retrospective review was performed to identify patients with available preoperative shoulder CT who subsequently underwent shoulder arthroplasty procedures at a single institution between 2015 and 2021. Data including age, sex, and smoking status were obtained. Radiology reports for CTs were reviewed for incidental findings and categorized based on location, tissue type, and/or body system. The rate of incidental findings and the rate at which further follow-up was recommended by the radiologist were determined.
Results
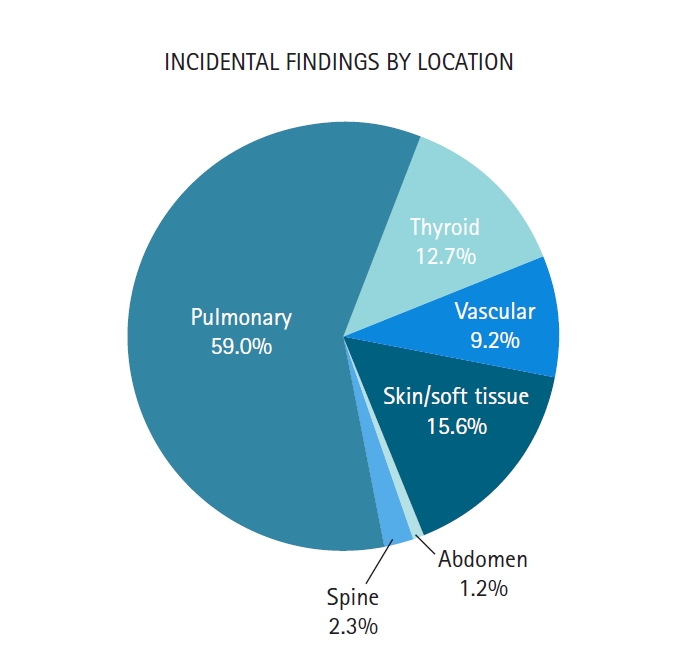
A total of 617 patients was identified. There were 173 incidental findings noted in 146 of these patients (23.7%). Findings ranged from pulmonary (59%), skin/soft tissue (16%), thyroid (13%), vascular (9%), spinal (2%), and abdominal (1%) areas. Of the pulmonary findings, 50% were pulmonary nodules and 47% were granulomatous disease. Overall, the final radiology report recommended further follow-up for 50% of the patients with incidental findings.
Conclusions
Incidental findings are relatively common in preoperative CTs obtained for shoulder arthroplasty, occurring in nearly one-quarter of patients. Most of these findings are pulmonary in nature. Overall, half of the patients with incidental findings were recommended for further follow-up. These results establish population data to guide orthopedic surgeons in patient counseling.
Level of evidence
III.
INTRODUCTION
Incidental imaging findings, commonly referred to as incidentalomas, are increasingly identified in advanced imaging studies. The increasing identification of such findings is likely due to a growth in the demand for advanced imaging studies as well as improvements in imaging [1]. This is particularly relevant to procedures in orthopedics for which advanced imaging is routinely obtained preoperatively. Specifically, it has become common practice to obtain computed tomography (CT) scans for preoperative planning/templating in the setting of anatomic total shoulder arthroplasty (TSA), reverse total shoulder arthroplasty (RSA), and even hemiarthroplasty (HA) [2-4]. Incidental findings commonly are reported by the reading radiologist in the final report. Improvements in resolution quality, coupled with the growing number of shoulder arthroplasty procedures performed every year in the United States [5-7], will likely contribute to an increased number of incidental findings. This poses a very specific challenge to surgeons, as they attempt to counsel patients on findings that may be unrelated to the underlying indication for a given imaging study.
There are many factors that may contribute to the challenge of incidental imaging findings to shoulder surgeons. First, there is limited study regarding the rate of incidental findings on preoperative shoulder CT scans performed prior to shoulder arthroplasty. Some of the available published research on this topic focuses on pulmonary images or aims to investigate incidental findings of different CT techniques [8,9]. The limited nature of the literature on this topic limit conversations with patients regarding the significance and prevalence of incidental findings, particularly those outside of the pulmonary system. Additionally, although shoulder CTs are windowed to include the entire glenohumeral joint, incidental findings may be noted within lung fields, the neck, the axilla, chest wall, and/or the brachium. Unfortunately, there can be wide variability with respect to the amount of adjacent fields included in shoulder CT scans. Thus, for example, the likelihood of an incidental lung nodule being identified on a given shoulder CT is highly dependent on how much of the lung field is included in the study. Furthermore, wide variability in the experience, training, and diligence of the reading radiologist may impact the rate at which incidental findings are noted, particularly when they are unrelated to the primary indication for that imaging study [10].
Another factor complicating the reporting of incidental findings to patients is that some orthopedic surgeons may not read the radiology report for imaging studies that they order. One study found that 20% of surveyed orthopedic surgeons indicated that they never read the radiology report for an X-ray study and 4% of surveyed orthopedic surgeons indicated that they never read the radiology report for CT scans [11]. The same study reported that only 19% of surveyed orthopedic surgeons always read the complete radiology report for X-ray studies and only 36% did so for CT scans [11]. Thus, even when incidental findings are noted by radiologists, these may go unreported to patients if surgeons are never aware of their existence. There are, of course, radiologists who communicate significant imaging findings with surgeons directly. However, there is significant variability in this process, which is dependent on the institution, radiologist, surgeon, and situation, among other factors.
Taken together, the issues highlighted above demonstrate the specific challenge of orthopedic surgeons when an incidental finding is noted on preoperative shoulder CT. Therefore, this study aims to identify and explore the incidence of incidental findings in CT scans performed for shoulder arthroplasty procedures and to assess the rate at which they warrant further follow-up.
METHODS
A retrospective study was conducted, for which Institutional Review Board of University of Iowa approval was obtained (#202103242). Informed consent was waived. Using an electronic medical record system, patients who had undergone anatomic TSA, RSA, or shoulder HA at a single institution between 2015 and 2021 were identified. Patients were identified utilizing current procedural terminology (CPT) codes for TSA or HA. Once these patients were identified, their medical records were reviewed, the procedure was confirmed, and all patients who had undergone a preoperative CT study of the operative shoulder were selected. For the purposes of this study, a preoperative CT was defined as one of the operative shoulder that had been performed within six months prior to the arthroplasty procedure. Patients who underwent a CT scan more than 6 months prior to surgery were excluded. Surgical indication or preoperative diagnosis were not utilized for inclusion or exclusion criteria in this study. Therefore, all patients that underwent TSA, RSA, or HA for fracture, primary glenohumeral osteoarthritis, or rotator cuff arthropathy, among other diagnoses, and who underwent a preoperative CT were included in this study. This generated a total cohort of 617 patients (Fig. 1).
The following demographic factors were collected for each patient based on review of each patient’s electronic medical record: age, sex, and smoking status at the time of surgery. The final radiology report for each preoperative shoulder CT was individually reviewed by the authors of this study. These radiology reports were categorized by presence or absence of incidental findings, generating two cohorts, one with incidental findings in their preoperative CT scans and another without incidental findings. For the purposes of this study, an incidental finding was defined as any finding noted in the final radiology report that was unrelated to the indication listed for the imaging study. Incidental findings were then sub-categorized based on tissue type, location, and/or organ system. These categories include pulmonary, skin/soft tissue, thyroid, vascular, spine, and abdominal areas. Given their predominance, pulmonary findings were further sub-classified based on finding type. Final radiology reports were reviewed for interpretation of the noted incidental findings as well as recommendations for further follow-up or work-up for that particular incidental finding. All CT images were acquired using a 0.6-mm collimator, which allows a spatial resolution less than 1 mm with matrix dimensions of 512×512 pixels. Shoulder images were reconstructed at 0.5×0.5 on this particular scanner utilizing dual energy. The scans were windowed by anatomical landmarks.
Statistical analysis of all collected data was performed using MATLAB (The MathWorks Inc.). Statistical significance was determined using a two-tailed Student t-test between two groups of continuous data (mean age) and a chi-square test to compare categorical values between two groups (sex and smoking status). Statistical significance was defined as P<0.05.
RESULTS
Patients were divided into cohorts of those with and those without incidental findings on preoperative CT scans. There were no statistical differences in age and sex between these two cohorts (P=0.152, P=0.111, respectively) (Table 1). These cohorts did differ significantly with respect to reported smoking status as patients with incidental findings on CT were more likely to be current smokers and less likely to be never smokers than patients without incidental findings on CT. In the cohort with incidental findings, 22.6% of patients were current smokers, compared to 14.0% in the cohort without incidental findings (P=0.021) (Table 1).
Of our total patient cohort of 617, there were 173 incidental findings noted in 146 patients (23.7%). These findings were noted in pulmonary (59.0%, 102/173), skin/soft tissue (15.6%, 27/173), thyroid (12.7%, 22/173), and vascular (9.2%, 16/173) areas. Less common were incidental findings involving the spine (2.3%) and abdomen (1.2%) (Fig. 2). The most commonly noted pulmonary findings were pulmonary nodules and granulomatous disease, representing 50.0% (51/102) and 47.1% (48/102) of pulmonary findings, respectively (Fig. 3). Further follow-up or work-up was recommended in the final radiology report for 73 of the 146 patients (50.0%) with incidental findings on preoperative shoulder CT. When the need for further follow-up was analyzed by type of incidental finding, radiologists suggested further follow-up for 47% (48/102) of pulmonary findings. Suggested types of follow-up included a dedicated chest CT for 34 patients (71%) and clinical correlation with medical and personal history for 14 patients (29%). In patients with an incidentally noted skin/soft tissue finding, 33% (9/27) required further follow-up comprising clinical correlation for six patients (66.7%), dedicated chest CT for two patients (22.3%), and a mammogram for one patient (1%). Radiologists recommended further follow-up for 65% (15/23) of patients with incidentally noted thyroid findings. An ultrasound was recommended for 14 (93.3%) of these patients and clinical correlation recommended for one (6.7%). Of the 16 vascular lesions noted, radiologists suggested further follow-up with a dedicated chest CT for only one patient (Fig. 4).
DISCUSSION
Incidental findings are commonly noted on advanced imaging studies. The data reported above demonstrate the commonality of these findings in preoperative shoulder CT scans obtained for shoulder arthroplasty. Based on our data, almost one-quarter of patients who undergo shoulder arthroplasty have incidental finding on preoperative shoulder CT. Even more surprising was the 50% rate at which radiologists recommended further follow-up or work up for patients with incidental findings. Therefore, one in eight patients undergoing shoulder arthroplasty have incidental findings on imaging warranting further work-up or evaluation. This represents a potentially large portion of a shoulder surgeon’s practice as well as a significant time commitment to appropriately and adequately counsel patients.
A large portion of the incidental findings identified in this study was pulmonary nodules. This is not surprising given the rate at which pulmonary nodules are incidentally noted on other imaging studies and the predicted prevalence with which they occur in the general population [12,13]. In fact, pulmonary nodules are common enough that guidelines exist for categorization based on need for further work-up, management, and risk of lung cancer [14,15]. There also exists literature in orthopedics pertaining to the identification of certain lung tumors, predominately with radiographs of the spine [16-18]. This literature may prove invaluable to the orthopedic surgeon and the radiologist with whom they collaborate as they counsel patients on incidentally identified pulmonary nodules.
One significant difference between cohorts identified in this study is that patients with incidental findings on CT were significantly more likely to be current smokers and significantly less likely to be never smokers than patients without incidental findings on CT. This finding is not particularly surprising given established associations between tobacco use and pulmonary pathology [19-21]. However, this is the only demographic factor of those evaluated that demonstrated significant difference between cohorts.
The rate of shoulder arthroplasty has increased significantly in recent decades and is projected to increase further [7,22-24]. This increase in shoulder arthroplasty has also contributed to multiple innovations, such as preoperative planning software and patient-specific implants and instrumentation [25,26]. In their current form, preoperative planning software platforms utilize three-dimensional reconstructions of two-dimensional shoulder CT scans [27]. Preoperative planning software can be utilized to calculate glenoid retroversion and humeral head subluxation with varying degrees of accuracy [2,28-30]. Preoperative planning software can aid in surgical preparation and implant selection for anatomic and reverse shoulder arthroplasty [31,32]. Advancements in preoperative planning software platforms have also contributed to an understanding of how component selection and implant positioning can influence impingement-free range of motion following reverse shoulder arthroplasty [33]. Given the potential benefits of preoperative planning software, it is expected that surgeons performing shoulder arthroplasty will be more likely to rely on preoperative CT scans. With the increased prevalence of shoulder arthroplasty and the increasing use of preoperative CT scans, it is very likely that incidental findings on shoulder CT scans will become a more common point of discussion for surgeons and patients prior to shoulder arthroplasty.
Although the literature is limited, previous studies have been published on incidental findings on shoulder CT. Most published studies have focused on pulmonary incidental findings or aimed to compare the incidence of these findings on different imaging techniques. Lopez et al. [8] demonstrated that 22.8% of patients undergoing TSA had pulmonary nodules incidentally detected on preoperative shoulder CT. Although this rate is similar to our reported overall rate of incidental findings (23.7%), the study by Lopez et al. [8] was limited to pulmonary nodules and did not account for alternative incidental findings. Thus, the rate of pulmonary nodules reported by Lopez et al. [8] is much higher than what was observed in our patient cohort, as only 59% of incidental findings were pulmonary in nature. Given our inclusion of all types of incidental findings, our study represents a valuable addition to the current literature on this subject. Another study by Chen et al. [9] assessed the rate of incidental findings and potentially pathologic incidental findings on shoulder CT. A primary goal of their study was to assess the rate of incidental findings on standard CT scans (2.5-mm slices) vs. thin-cut CT scans (1.25-mm slices). Interestingly, they demonstrated a rate of incidental findings in their standard CT scan group (22%) similar to the rate reported in our study (23.7%). However, Chen et al. [9] found that only 15.6% of incidental findings on CT scans were classified as “potentially pathologic.” This rate is substantially lower than the 50% rate at which incidental findings warrant further work-up according to our study. Multiple possible explanations exist for this disparity including the specific definition used for “potentially pathologic,” differences in patient populations, and variability in the interpretations of the radiologists reading these CT scans.
There are limitations of our study. This study was performed retrospectively and is limited by the biases inherent to retrospective studies. Selection bias may play a role in our results as only patients who went on to undergo shoulder arthroplasty were included in this study. There may have been patients who had been indicated for such a procedure, had undergone preoperative shoulder CT, and did not ultimately undergo the surgical procedure. It is also possible that some of these patients may have chosen to forego arthroplasty or been deemed to not be candidates for arthroplasty secondary to a condition related to an incidental imaging finding. However, this is not discernable given our methodology. Given that the patients included in this study were treated at an academic tertiary medical center, the possibility exists that our patient cohort is not representative of the general population, particularly with regard to demographic factors. Finally, original radiology reports were reviewed for incidental findings, and we did not reinterpret the included images. Therefore, the possibility exists that there are additional incidental findings that were not originally identified by the radiologists and are thus not included in this data. However, we would argue that this more accurately reflects the clinical scenario in which incidental findings are typically identified and reported, as radiologists are not alerted to “look for” incidental findings specifically for the purpose of a study. Thus, we would consider this method a strength of the study, as it allows us to minimize confirmation bias.
The goal of this study was to evaluate the incidence of incidentally noted findings on preoperative shoulder CT for shoulder arthroplasty. Our hope is that this information can help orthopedic surgeons in considering the likelihood of encountering an incidental finding and, above all, to help guide them in counseling affected patients.
CONCLUSIONS
Incidental findings are commonly noted in imaging studies and could be found in about one-quarter of patients undergoing shoulder arthroplasty. Furthermore, half of incidental images might warrant further follow-up. The findings of this study provide useful information for orthopedic surgeons counseling patients regarding incidental imaging findings unrelated to the primary purpose of imaging study prior to shoulder arthroplasty. This study represents an important addition to the literature to help guide orthopedic surgeons as they counsel patients regarding incidental imaging findings.
Notes
Author contributions
Conceptualization: DGM, JVN, BMP. Data curation: DGM, MFB, TDH, JC. Investigation: DGM, MFB, JC. Methodology: MFB, JVN, BMP. Project administration: BMP. Supervision: MFB, BMP. Validation: JC. Writing – original draft: DGM. Writing – review & editing: MFB, TDH, JVN, BMP.
Conflict of interest
BMP has the following financial disclosures listed in the Funding section. No other potential conflicts of interest relevant to this article were reported.
Funding
BMP received research funding from Stryker Orthopedics and is a paid consultant for Stryker Orthopedics.
Data availability
Contact the corresponding author for data availability.
Acknowledgments
None.