Anatomic factors associated with degeneration and fraying of the coracoacromial ligament
Article information
Abstract
Background
The coracoacromial ligament (CAL) is frequently observed to be damaged during arthroscopy and it is unclear how demographic, anatomic, and radiographic factors are related to CAL degeneration in full-thickness rotator cuff tears.
Methods
A prospective study was conducted of patients at a single institution undergoing shoulder arthroscopy for first-time, full-thickness rotator cuff tears. We evaluated preoperative anteroposterior radiographs to obtain critical shoulder angle, glenoid inclination, acromial index, acromiohumeral distance, lateral acromial angle, and acromial morphology. We documented CAL quality, rotator cuff tear size and pattern during arthroscopy. Multiple logistic regression was used to identify predictive factors for encountering severe CAL fraying during arthroscopy.
Results
Shoulders had mild CAL degeneration in 58.1% of cases, whereas severe CAL degeneration was present in 41.9% of shoulders. Patients with severe CAL attrition were significantly older (62.0 years vs. 58.0 years, P=0.042). Shoulders with severe CAL attrition had large rotator cuff tears in 54.1% of cases (P<0.001), and tears involving the infraspinatus (63.2% vs. 29.6%, P=0.003). The severe degeneration group was more likely to have a larger critical shoulder angle measurement on preoperative radiographs than those in the mild attrition group (36.1°±3.6° [range, 30°–45°] vs. 34.1°±3.8° [range, 26°–45°], P=0.037).
Conclusions
While the clinical impact of CAL degeneration remains uncertain, increased severity of CAL degeneration is associated with older age, larger rotator cuff tear size, presence of infraspinatus tearing, and increased preoperative critical shoulder angle.
Level of evidence
III.
INTRODUCTION
The coracoacromial ligament (CAL) is a thickened band of fibrous tissue that extends from the anterolateral margin of the acromion to the base of the coracoid, along the anterior aspect of the capsule between the supraspinatus and subscapularis tendons in the shoulder [1]. It most commonly exists as distinct posteromedial and anterolateral bands. The anterolateral band is generally thicker, more commonly associated with spurring, and is thought to act as a load-bearing structure in the shoulder [2]. As part of the coracoacromial arch, the CAL has been suggested to contribute to restraint of anterosuperior humeral head displacement [3,4], in addition to having a potential role in shoulder biomechanics, stability, and proprioception [5,6].
Patients with degenerative changes of the CAL are more likely to have acromial undersurface changes, such as enthesophyte formation at the site of CAL insertion, and these changes may play a role in subacromial impingement [5]. Neer famously reported on mechanical impingement of the tendinous rotator cuff on the anterior third of the acromion and the CAL. He subsequently recommended resection of the undersurface of the anterior acromion and detachment of the CAL in symptomatic patients [7].
It remains unknown whether CAL tearing is related to intrinsic degeneration or extrinsic impingement factors like variations in bony anatomy or altered shoulder mechanics due to rotator cuff disease. The relationship between bursal-sided partial-thickness rotator cuff tears (RCTs) and CAL fraying has been demonstrated [8]. The aim of the present study was to determine demographic, anatomic, and radiographic factors associated with CAL degeneration and tearing in patients undergoing surgery for full-thickness RCTs. We hypothesized that CAL degeneration would be associated with greater tear size.
METHODS
Participants
This study received approval from the Institutional Review Board under Federalwide Assurance (No. 00002109). Informed consent was obtained from all patients. We performed an institutional review board-approved prospective study of consecutive patients undergoing shoulder arthroscopy for full-thickness RCTs by two fellowship-trained shoulder surgeons at a single institution (SG, SN). All procedures included diagnostic arthroscopy. Patients with a history of prior surgery, fracture, or infection on the ipsilateral shoulder were excluded, as were those without preoperative plain radiographs and those over the age of 80 years. Demographic, radiographic, and intraoperative data were collected.
Data and Measurements
The quality of the CAL, size and pattern of the RCT, and presence of biceps tendon pathology were recorded at the time of diagnostic arthroscopy. CAL quality was graded according to the Copeland-Levy classification of acromial lesions (Table 1), which has been shown to have excellent intra- and inter-observer reliability [9]. For the purpose of our study, grades 0 and 1 were considered to represent minor CAL degeneration, whereas grades 2–3 represented severe CAL degeneration. RCT size and pattern were described according to the DeOrio and Cofield Classification [10] and Ellman systems [11], respectively.
Preoperative radiographic parameters were measured on available anteroposterior (AP) radiographs and included the critical shoulder angle (CSA), glenoid inclination (Gin), acromial index (AI), acromiohumeral distance (AHD), lateral acromial angle (LAA), and acromial morphology. All measurements were performed by a single fellowship-trained shoulder surgeon who was blinded to all intraoperative findings, including CAL degeneration grade. CSA was measured as the angle between the line connecting the superior and inferior margins of the glenoid and the line connecting the inferior margin of the glenoid to the lateral border of the acromion [12]. To determine Gin, the β angle was first measured between the line connecting the superior and inferior margins of the glenoid and the line tangential to the base of the supraspinatus fossa. Gin was subsequently calculated as the difference between 90 degrees and the β angle [13]. AI was determined by dividing the horizontal distance from the glenoid plane to the lateral aspect of the proximal humerus by the distance from the glenoid plane to the lateral border of the acromion [14]. AHD defined the shortest vertical distance between the inferior aspect of the acromial undersurface and the most superior portion of the humeral head [15]. The LAA was recorded as the angle between the line parallel to the acromial undersurface and the line connecting the superior and inferior margins of the glenoid [16]. Acromial morphology was classified as initially described by Bigliani et al. [17] with type I being flat, type II curved, and type III hooked.
Statistical Analysis
Intraoperative CAL quality was the dependent variable in this study. Continuous variables were summarized using sample means with standard deviations and compared between groups with t-tests or Mann-Whitney U-tests to determine the significance of differences, as appropriate. Categorical data are presented as percentages, and the significance of differences in these variables between groups was assessed using chi-square or Fisher’s exact tests. Statistical significance was set at P<0.05. A multiple logistic regression model was implemented to estimate the probability of severe CAL degeneration during arthroscopic evaluation. Variables chosen for this regression analysis included patient age, tear size, torn tendon, and preoperative CSA and AHD measurements based on significance in univariate analysis.
RESULTS
Among the 93 patients included in this study, mean age was 59±8 years, and surgery was performed on the dominant extremity in 53 (57.0%). At the time of diagnostic arthroscopic evaluation, 20 (21.5%) CA ligaments were classified as grade 0 degeneration, 34 (36.6%) as grade 1, 29 (31.2%) as grade 2, and 10 (10.8%) as grade 3. Mild CAL degeneration (grades 0–1) was seen in 54 shoulders (58.1%), whereas severe CAL degeneration (grades 2–3) was seen in 39 (41.9%). Patients with severe CAL attrition were significantly older than those with mild CAL attrition (62.0 years vs. 58.0 years, P=0.042). Arm dominance was not correlated with severity of CAL degeneration.
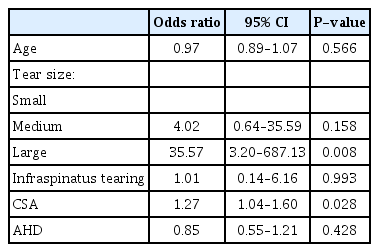
Rotator cuff tear size was associated with increasing severity of CAL degeneration, with 54.1% of shoulders with severe CAL attrition having concomitant large RCTs (P<0.001) (Table 2). Only 17 of 59 shoulders (28.8%) with small or medium-sized tears had severe CAL degeneration, as opposed to 20 of 28 shoulders (71.4%) with large-sized tears. Multivariate regression demonstrated that patients with large tears were 35.6 times more likely to have concurrent severe CAL degeneration than those with small tears (P=0.008) (Table 3). Furthermore, RCTs involving the infraspinatus were more frequent in patients with severe CAL degeneration than in those with mild changes (63.2% vs. 29.6%, P=0.003) (Table 2).
Shoulders with severe CAL degenerative changes trended toward U-shaped tears compared to shoulders with mild CAL changes (25.7% vs. 9.6%), although this finding did not reach statistical significance (P=0.088) (Table 2). Similarly, severe CAL degeneration trended toward a higher likelihood of RCT tendon retraction than shoulders with mild CAL changes (82.1% vs. 63.0%), although this too did not reach statistical significance (P=0.077). The status of the subscapularis and long head biceps tendon was not associated with severity of CAL degeneration.
Radiographically, patients in the severe attrition group were more likely to have larger CSA measurements on preoperative radiographs than those in the mild attrition group (36.1°±3.6° [range, 30°–45°] vs. 34.1°±3.8° [range, 26°–45°], P=0.037). Differences in Gin, AHD, LAA, AI, and acromial morphology were not significantly different between groups (Table 4).
DISCUSSION
CAL degeneration is commonly encountered during arthroscopic rotator cuff repair. While the clinical relevance of CAL degeneration and the need to address it surgically are unclear, this study serves as an early step in understanding the nature of this arthroscopic finding. The present study suggests that age, RCT size, and preoperative radiographic CSA measurement are associated with CAL degeneration.
As may be expected with other degenerative changes in the shoulder, patients with more severe CAL attrition were significantly older than those with mild changes. Rothenberg et al. [5] proposed that such age-dependent changes may be due to chronic stress as well as cellular degradation, with subsequent thickening and stiffening contributing to capsular tightness, rotator cuff pathology, and impingement. Furthermore, when combined with radiographic analysis, Moor et al. [18] found that patients with full-thickness RCTs were significantly older and had larger CSA measurements than those with intact rotator cuffs. Despite this, Ogata and Uhthoff [19] found no correlation between aging and acromial undersurface degenerative changes in their cadaveric study, postulating that RCTs are unlikely to be initiated by impingement. However, these results by Ogata and Uhthoff [19] were not replicated in our study; rather, we observed a correlation between increased acromial undersurface changes and patient age.
Large RCTs were associated with increased severity of CAL degeneration, as was the presence of infraspinatus tendon tearing. In evaluating the relationship between CAL attrition and partial-thickness RCTs, Kanatli et al. [8] found that only 4.1% of shoulders with partial-thickness RCTs had grade 3 CAL degeneration, corroborating the idea that grade 3 changes likely exist with concomitant full-thickness tears. Larger tears render a bare greater tuberosity, which may contact the acromial undersurface in abduction and lead to CAL tearing. Regarding tear location, biomechanical cadaveric studies have previously emphasized the importance of the posterosuperior cuff, where tear extension involving the infraspinatus leads to altered force coupling and shoulder joint mechanics, including superior humeral head translation [20,21]. This may explain our finding that severe CAL attrition is more likely to be associated with infraspinatus tearing, given the potential for increased load on the CAL due to altered biomechanics.
Among the radiographic measurements analyzed in our study, only CSA had a statistically significant association with CAL findings, with increased CAL degenerative changes having a higher CSA. CSA incorporates lateral acromial extension and Gin, and increased CSA has been associated with rotator cuff tearing in several studies [12,18,22,23]. This has been theorized to result from an increase in shear force from the vector of the deltoid’s pull, which results in superior migration of the proximal humerus and increased load of the rotator cuff [4,24]. This same mechanism may increase the load on the coracoacromial arch and CAL, contributing to increased attritional wear. Still, other studies have called into question the association between CSA and RCTs [25,26]. Kim et al. [27] recently suggested that RCTs were associated more strongly with the presence of subacromial osteophytes than with CSA measurement. Oh et al. [28]suggested that acromial spurring forms by traction of the CAL and is related to rotator cuff tearing. This could further support our finding of the association between CAL attrition severity and increasing RCT size.
This study methodology does have several limitations. Radiographic measurements are subject to inaccuracy due to factors including beam projection and vector, and the position of the patient’s scapula can affect the overall quality of the AP shoulder X-ray and influence measurements. In the absence of adequate pre-existing data to support a true power analysis, we planned to enroll a minimum of 80 patients. Because of this, nonsignificant results may be influenced by type II error. Finally, given that only the performing surgeon performed intraoperative CA ligament grading and radiographic measurements, the inter-rater reliability of CA ligament grading or radiographic measurement could not be assessed.
CONCLUSIONS
While the CAL role in the coracoacromial arch as a load-bearing stabilizer has been well-studied, both the clinical impact of CAL degeneration and surgical role of acromioplasty and CAL release remain uncertain. We found that increased severity of CAL degeneration is associated with increased patient age, larger RCT size, presence of infraspinatus tearing, and increased preoperative CSA. Further studies are needed to guide clinical decision-making regarding the intraoperative management of RCTs with concomitant CAL degeneration and tearing.
Notes
Author contributions
Conceptualization: JS, MG, TN, SN. Data curation: RL, JS, MG, TN, SG, SN. Formal analysis: RL, JS, MG, TN, SG, SN. Project administration: TN, SN. Supervision: TN, SG, SN. Visualization: RL, MG Writing – original draft: RL, JS, MG, TN, S Gates, SN. Writing – review & editing: RL, JS, MG, TN, SG, SN.
Conflict of interest
None.
Funding
None.
Data availability
Contact the corresponding author for data availability.
Acknowledgments
None.