1. Gaskill TR, Taylor DC, Millett PJ. Management of multidirectional instability of the shoulder. J Am Acad Orthop Surg 2011;19:758â67.


2. Millett PJ, Clavert P, Hatch GF, Warner JJ. Recurrent posterior shoulder instability. J Am Acad Orthop Surg 2006;14:464â76.


3. Provencher MT, Midtgaard KS, Owens BD, Tokish JM. Diagnosis and management of traumatic anterior shoulder instability. J Am Acad Orthop Surg 2021;29:e51â61.


5. Owens BD, Campbell SE, Cameron KL. Risk factors for anterior glenohumeral instability. Am J Sports Med 2014;42:2591â6.


6. Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med 2007;35:1168â73.


8. Hill HA, Sachs MD. The grooved defect of the humeral head. Radiology 1940;35:690â700.

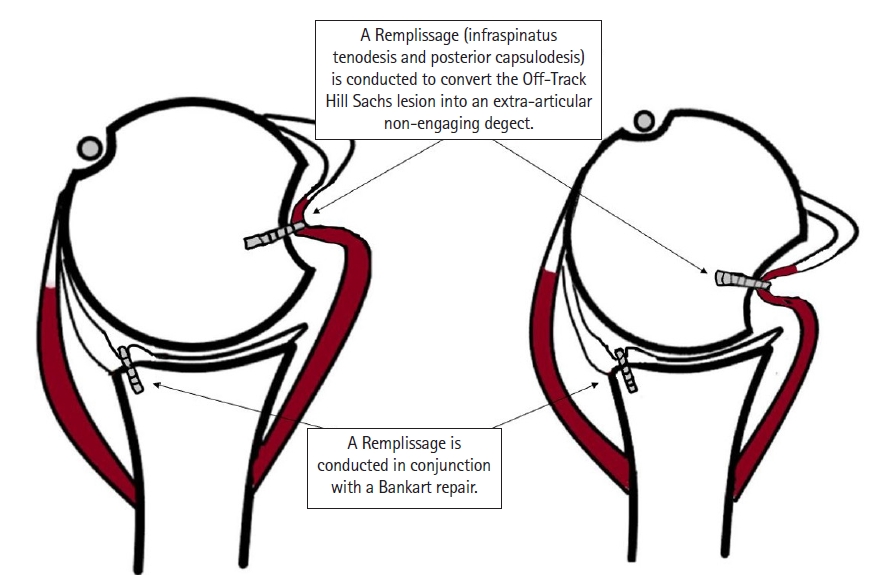
9. Buza JA, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill-Sachs remplissage: a systematic review. J Bone Joint Surg Am 2014;96:549â55.

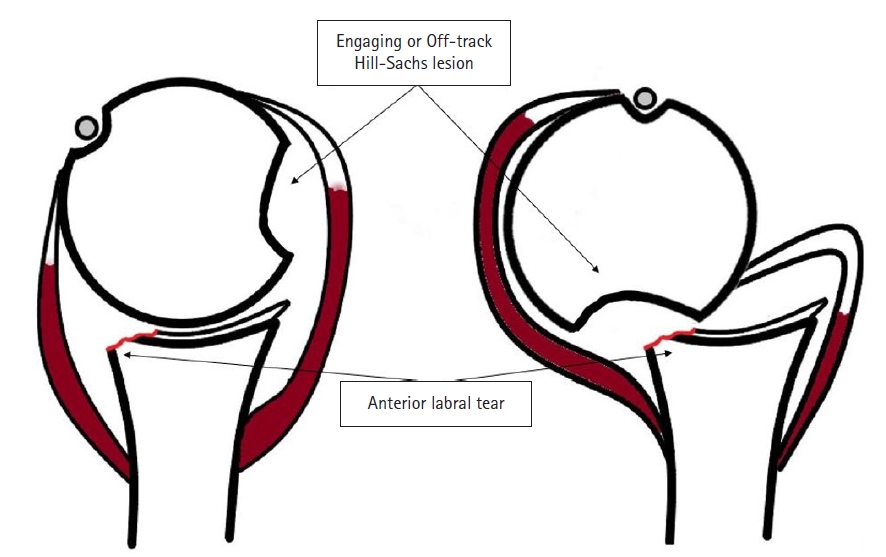
10. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677â94.

11. Palmer I, Widen A. The bone block method for recurrent dislocation of the shoulder joint. J Bone Joint Surg Br 1948;30:53â8.


12. Armitage MS, Faber KJ, Drosdowech DS, Litchfield RB, Athwal GS. Humeral head bone defects: remplissage, allograft, and arthroplasty. Orthop Clin North Am 2010;41:417â25.


13. Chapovsky F, Kelly JD. Osteochondral allograft transplantation for treatment of glenohumeral instability. Arthroscopy 2005;21:1007.


14. Hawkins RJ, Angelo RL. Glenohumeral osteoarthrosis: a late complication of the Putti-Platt repair. J Bone Joint Surg Am 1990;72:1193â7.


15. Kazel MD, Sekiya JK, Greene JA, Bruker CT. Percutaneous correction (humeroplasty) of humeral head defects (Hill-Sachs) associated with anterior shoulder instability: a cadaveric study. Arthroscopy 2005;21:1473â8.


16. Kropf EJ, Sekiya JK. Osteoarticular allograft transplantation for large humeral head defects in glenohumeral instability. Arthroscopy 2007;23:322.

17. Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR. The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther 2006;36:138â51.


18. Weber BG, Simpson LA, Hardegger F. Rotational humeral osteotomy for recurrent anterior dislocation of the shoulder associated with a large Hill-Sachs lesion. J Bone Joint Surg Am 1984;66:1443â50.


19. Yagishita K, Thomas BJ. Use of allograft for large Hill-Sachs lesion associated with anterior glenohumeral dislocation: a case report. Injury 2002;33:791â4.


20. Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-sachs "remplissage": an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy 2008;24:723â6.


21. Alkaduhimi H, Verweij LP, Willigenburg NW, van Deurzen DF, van den Bekerom MP. Remplissage with Bankart repair in anterior shoulder instability: a systematic review of the clinical and cadaveric literature. Arthroscopy 2019;35:1257â66.


22. Lazarides AL, Duchman KR, Ledbetter L, Riboh JC, Garrigues GE. Arthroscopic remplissage for anterior shoulder instability: a systematic review of clinical and biomechanical studies. Arthroscopy 2019;35:617â28.


23. Liu JN, Gowd AK, Garcia GH, Cvetanovich GL, Cabarcas BC, Verma NN. Recurrence rate of instability after remplissage for treatment of traumatic anterior shoulder instability: a systematic review in treatment of subcritical glenoid bone loss. Arthroscopy 2018;34:2894â907.


24. Wolf EM, Pollack ME. Hill-Sachs âRemplissageâ: an arthroscopic solution for the engaging Hill-Sachs lesion (SS-32). Arthroscopy 2004;20(Suppl 1):E14â5.

25. Hurley ET, Toale JP, Davey MS, et al. Remplissage for anterior shoulder instability with Hill-Sachs lesions: a systematic review and meta-analysis. J Shoulder Elbow Surg 2020;29:2487â94.


26. Flower WH. On the pathologic changes produced in the shoulder joint by traumatic dislocation as derived from an examination of all the specimens illustrating this Injury in the Museums of London. Trans Path Soc Lond 1861;12:179â201.
27. Polio W, Brolin TJ. Remplissage for anterior shoulder instability: history, indications, and outcomes. Orthop Clin North Am 2022;53:327â38.

28. Connolly J. Humeral head defects associated with shoulder dislocation: their diagnostic and surgical significance. Instr Course Lect 1972;2:210â8.
29. Provencher MT, Frank RM, Leclere LE, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg 2012;20:242â52.


31. Grimberg J, Diop A, Bou Ghosn R, Lanari D, Canonne A, Maurel N. Bankart repair versus Bankart repair plus remplissage: an in vitro biomechanical comparative study. Knee Surg Sports Traumatol Arthrosc 2016;24:374â80.


32. Cho NS, Yoo JH, Rhee YG. Management of an engaging Hill-Sachs lesion: arthroscopic remplissage with Bankart repair versus Latarjet procedure. Knee Surg Sports Traumatol Arthrosc 2016;24:3793â800.


33. Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 2007;16:649â56.


34. Omori Y, Yamamoto N, Koishi H, et al. Measurement of the glenoid track in vivo as investigated by 3-dimensional motion analysis using open MRI. Am J Sports Med 2014;42:1290â5.


36. Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy 2014;30:90â8.


37. Yang JS, Mehran N, Mazzocca AD, Pearl ML, Chen VW, Arciero RA. Remplissage versus modified latarjet for off-track Hill-Sachs lesions with subcritical glenoid bone loss. Am J Sports Med 2018;46:1885â91.


38. Garcia GH, Degen RM, Bui CN, McGarry MH, Lee TQ, Dines JS. Biomechanical comparison of acute Hill-Sachs reduction with remplissage to treat complex anterior instability. J Shoulder Elbow Surg 2017;26:1088â96.


39. Bishop JY, Hidden KA, Jones GL, Hettrich CM, Wolf BR, MOON Shoulder Group. Factors influencing surgeon's choice of procedure for anterior shoulder instability: a multicenter prospective cohort study. Arthroscopy 2019;35:2014â25.


40. Haroun HK, Sobhy MH, Abdelrahman AA. Arthroscopic Bankart repair with remplissage versus Latarjet procedure for management of engaging Hill-Sachs lesions with subcritical glenoid bone loss in traumatic anterior shoulder instability: a systematic review and meta-analysis. J Shoulder Elbow Surg 2020;29:2163â74.


41. Garcia GH, Wu HH, Liu JN, Huffman GR, Kelly JD. Outcomes of the remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med 2016;44:1124â30.


42. Ding Z, Cong S, Xie Y, Feng S, Chen S, Chen J. Location of the suture anchor in Hill-Sachs lesion could influence glenohumeral cartilage quality and limit range of motion after arthroscopic Bankart repair and remplissage. Am J Sports Med 2020;48:2628â37.


43. Martinez-Catalan N, Kazum E, Zampeli F, Cartaya M, Cerlier A, Valenti P. Long-term outcomes of arthroscopic Bankart repair and Hill-Sachs remplissage for bipolar bone defects. Eur J Orthop Surg Traumatol 2023;33:947â53.


45. Han F, Chin BY, Tan BH, Lim CT, Kumar VP. Clinical outcomes of the reverse McLaughlin procedure for Hill-Sachs lesions in anterior shoulder instability. J Orthop Surg (Hong Kong) 2019;27:2309499018816444.


48. Bastard C, Herisson O, Gaillard J, Nourissat G. Impact of remplissage on global shoulder outcome: a long-term comparative study. Arthroscopy 2019;35:1362â7.


49. Brilakis E, Avramidis G, Malahias MA, et al. Long-term outcome of arthroscopic remplissage in addition to the classic Bankart repair for the management of recurrent anterior shoulder instability with engaging Hill-Sachs lesions. Knee Surg Sports Traumatol Arthrosc 2019;27:305â13.


50. Pandey V, Gangadharaiah L, Madi S, et al. A retrospective cohort analysis of arthroscopic Bankart repair with or without remplissage in patients with off-track Hill-Sachs lesion evaluated for functional outcomes, recurrent instability, and range of motion. J Shoulder Elbow Surg 2020;29:273â81.


51. Feng S, Li H, Chen Y, Chen J, Ji X, Chen S. Bankart repair with remplissage restores better shoulder stability than Bankart repair alone, and medial or two remplissage anchors increase stability but decrease range of motion: a finite element analysis. Arthroscopy 2022;38:2972â83.


52. Davis WH, DiPasquale JA, Patel RK, et al. Arthroscopic remplissage combined with Bankart repair results in a higher rate of return to sport in athletes compared with Bankart repair alone or the Latarjet procedure: a systematic review and meta-analysis. Am J Sports Med 2023;3635465221138559.

53. Gouveia K, Harbour E, Athwal GS, Khan M. Return to sport after arthroscopic Bankart repair with remplissage: a systematic review. Arthroscopy 2023;39:1046â59.


54. Gouveia K, Abidi SK, Shamshoon S, et al. Arthroscopic Bankart repair with remplissage in comparison to bone block augmentation for anterior shoulder instability with bipolar bone loss: a systematic review. Arthroscopy 2021;37:706â17.


55. Paul RW, Reddy MP, Sonnier JH, et al. Increased rates of subjective shoulder instability after Bankart repair with remplissage compared to Latarjet surgery. J Shoulder Elbow Surg 2023;32:939â46.