Minimally invasive distal biceps tendon repair: a case series
Article information
Abstract
Background
Distal biceps tendon repairs are commonly performed using open techniques. A minimally invasive distal biceps tendon repair technique using a speculum and hooded endoscope was developed to improve visualization, reduce soft-tissue dissection, and minimize complications. This paper describes the technique and reports the outcomes of 75 minimally invasive distal biceps tendon repairs.
Methods
The operation reports and outcomes of 75 patients who underwent distal biceps tendon repair using this technique between 2011 and 2021 were retrospectively reviewed.
Results
Median time to follow-up was 12 months (interquartile range [IQR], 6–56 months). Primary outcomes were function as measured by the Disabilities of Arm, Shoulder and Hand Score (DASH) questionnaire, and rate of complications. Median DASH score was 1.7 of 100 (IQR, 0–6.8). There were 2 of 75 (2.7%) re-ruptures of the distal tendon. There were no cases of vascular injury, proximal radius fracture, or posterior interosseous nerve, median, or ulnar nerve palsy.
Conclusions
In this series, minimally invasive distal biceps repair was safe and effective with a low rate of major complications. Recovery of function, as indicated by low DASH scores, was satisfactory, and inconvenience during recovery was minimized.
Level of evidence
IV.
INTRODUCTION
Distal biceps tendon (DBT) ruptures account for nearly 10% of all biceps tendon ruptures [1-4], with an incidence of 2.55 per 100,000 patients per year reported in the US [5]. The majority occur in men between 40 and 60 years old, with a greater incidence among manual workers, weight-lifters, and athletes [3,6]. Recent epidemiological studies found a similar prevalence between dominant and non-dominant arms [7]. The mechanism of injury is commonly a rapid unanticipated eccentric extension force to the flexed elbow. The tendon is typically avulsed from its distal insertion as an acute event, but pre-existing degeneration is likely to contribute to a large proportion of tears [8].
Although nonoperative treatment may be an option in older, low-demand patients with comorbidities, surgical repair optimizes recovery of flexion and supination strength and allows improved cosmesis [9,10]. Advancements in the biomechanical strength of repair constructs have allowed earlier and less intrusive rehabilitation without a corresponding increase in adverse events [11-13]. The cortical button was first applied to repair of the DBT by Bain in 1995 [14] and has the advantages of simplicity, ease of deployment, limited exposure and avoids blind suturing deep in the forearm [12,14,15], Bain et al. [16] describe “prefabrication,” in which the tendon is sutured to the button outside of the wound, and then advanced and locked into position. Preparation of the radial tuberosity is the only aspect of the surgery performed deep in the forearm [17].
Endoscopically assisted or fully endoscopic approaches to DBT repair have been developed with the aim of improving visualization and have utility in both evaluation and repair of injured tendons [9,10]. Use of an endoscope facilitates retrieval and repair of the tendon via a small single anterior incision, allowing a clear and magnified view [18]. Dissection and retraction of tissues is minimized, reducing the risk of iatrogenic injury to neurovascular structures and resulting in a smaller scar [9,19,20]. Additional portals allow safe access to proximal and distal regions if required [15]. Tendinopathy, bursitis and partial tears can be difficult to diagnose clinically, with a conventional magnetic resonance imaging (MRI) sensitivity of less than 60% [21]. Consequently, endoscopy is helpful in evaluation of tendinosis or partial tears [7]. Endoscopic visualization also permits controlled tendon retrieval, footprint preparation, and precise placement of the fixation device [22]. Although small series have shown outcomes comparable to open techniques, some endoscopic DBT repair techniques are technically difficult and potential remains for injury to neurovascular, musculotendinous and osseous structures [10,21]. Anatomic variation in neurovascular structures has been observed, and systematic identification and protection of the lateral antebrachial cutaneous nerve (LABCN) of the forearm is advised [10]. Endoscopic repair is also time-sensitive, as lengthy irrigation causes swelling of the bursa, impairing the view and precluding further endoscopic treatment [22].
This study aims to describe a surgical technique for minimally invasive DBT repairs, where the ruptured tendon is identified and retrieved using an endoscope but the remainder of the operation is performed under direct vision with a speculum used for retraction. It has sufficient similarity to open repairs to allow easy adoption and recommendations to address the learning curve and progression to more difficult cases are provided. To the best of our knowledge, this is the largest reported case series of minimally invasive DBT repairs to date.
METHODS
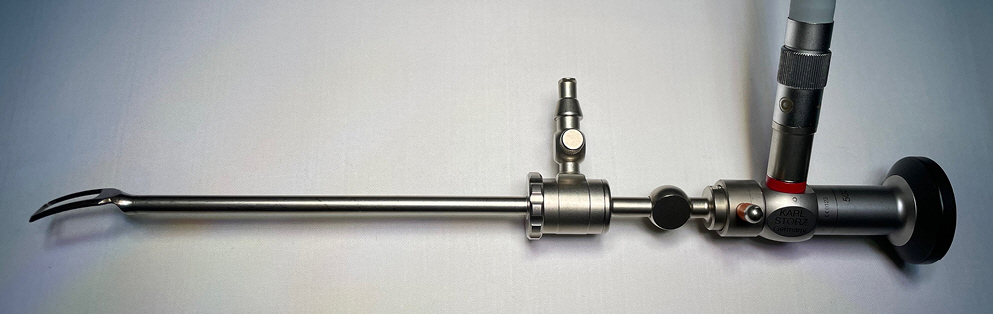
A search of the authors’ patient database (Genie Solutions) was performed to identify all patients who had undergone minimally invasive surgical repair of DBT tears between January 1, 2011, and July 31, 2021. Written informed consent was obtained from all patients for their anonymized information to be published. Ethics approval was not sought for the present study because it is a retrospective case audit. Exclusion criteria included the use of tendon grafts, concurrent repair of additional structures at the elbow, and revision surgery. In total, 94.7% of patients (n=71) were male, and 57.3% (n=43) of cases involved the dominant arm (Table 1). Mean age was 48.7 years (range, 22–75 years). All surgeries included occurred at least 6 months prior to data analysis. All preoperative evaluations and surgeries were conducted by one experienced specialist orthopedic upper limb surgeon. Follow-up evaluation was completed by the same surgeon, a clinical nurse specialist, and specialized upper limb therapists.
Diagnosis was based on history and physical examination, with additional imaging to support diagnosis arranged either by the referring doctor or specialist surgeon. Ultrasound examination was performed in 92% (69/75) of cases, MRI in 40% (30/75), and X-ray in 16% (12/75). The Disabilities of Arm, Shoulder and Hand Score (DASH) questionnaire was used to assess self-reported function, with higher scores out of 100 indicating greater disability. Paraesthesia was assessed subjectively, with all patients questioned regarding sensory disturbance at follow-up. Postoperative radiographs were not routinely taken. Active range of motion was not a primary outcome of interest and was formally measured with a goniometer if deficits were observed.
Surgical Technique
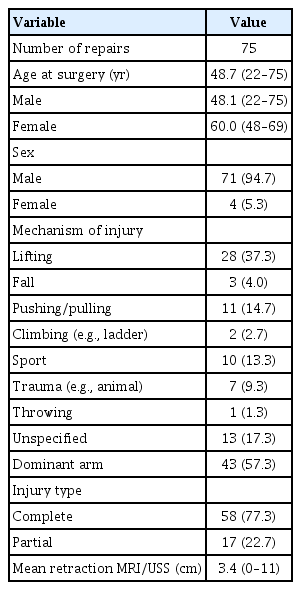
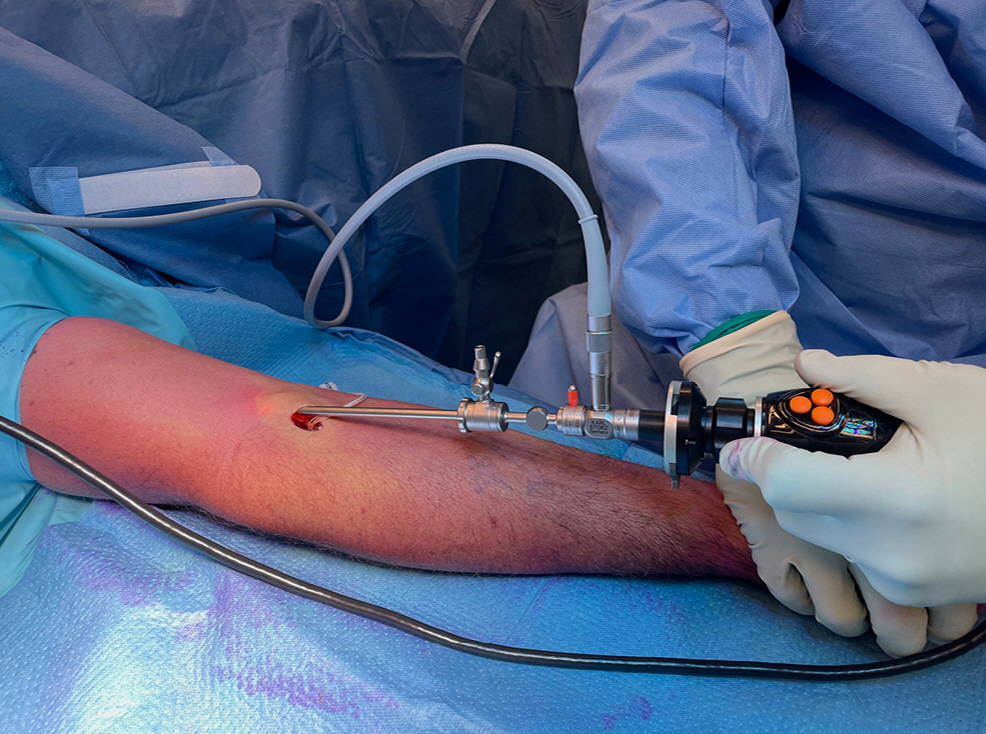
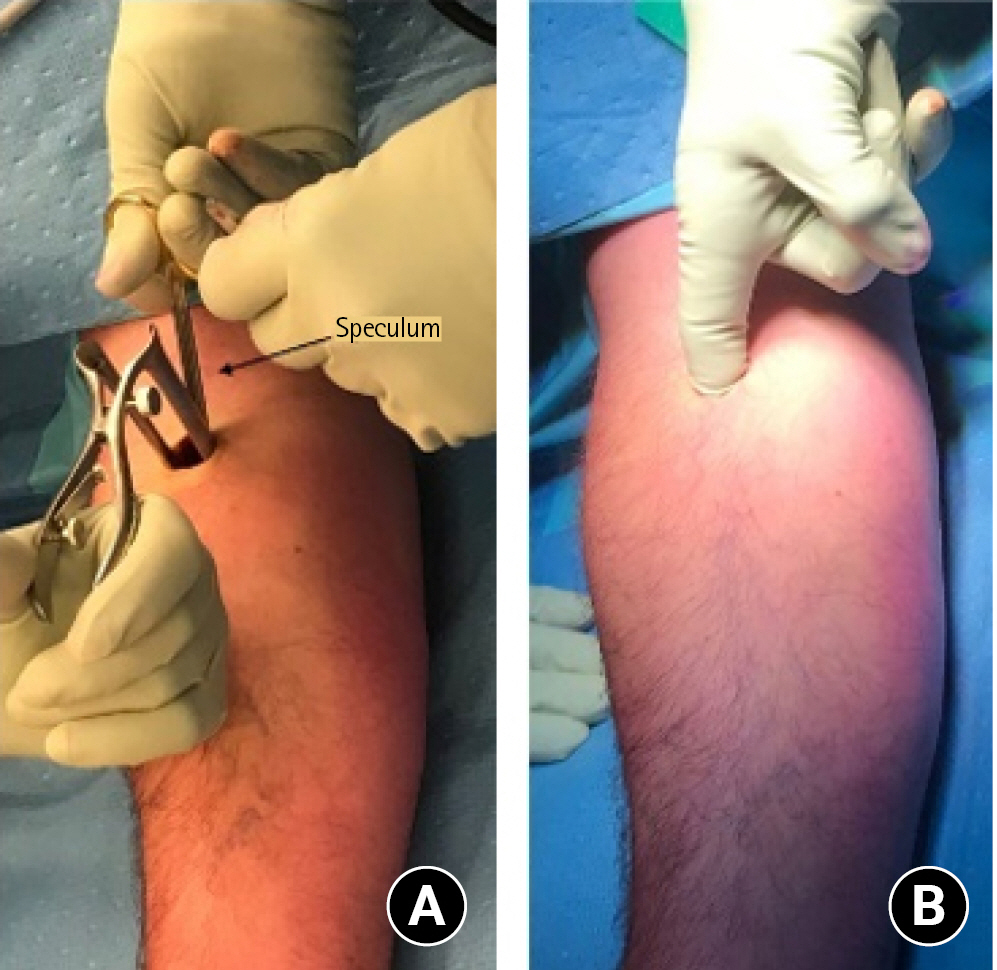
The procedure is undertaken under general or regional anesthesia with the upper limb on an arm table and an arm tourniquet inflated to 250 mmHg. A Karl Storz Hopkins wide-angle Forward-Oblique telescope with an optical dissector (Fig. 1), distal spatula, and Cottle speculum (Fig. 2) are utilized during the procedure. The senior author uses loupe magnification during the procedure.
With the forearm supinated, a 2-cm volar longitudinal incision is created commencing approximately 5-cm distal to the elbow crease, just medial to the extensor wad. The fascia is incised, and the LABCN of the forearm is identified and protected. The radial tuberosity is located using blunt dissection (Fig. 3A) and digital palpation (Fig. 3B). The speculum is used at this stage as the sole retractor; it allows excellent visualization of the tuberosity using the operating light directly overhead, or alternatively a head-mounted light or speculum light. The speculum position is progressively altered towards the radial tuberosity until the positioning is perfect. Use of the speculum prevents excessive tension on the local neurovascular structures or compression of the posterior interosseous nerve (PIN), which can occur if a retractor is placed around the side of the radius. Any DBT remnants attached to the tuberosity and prominent areas of the distal biceps bursa are debrided using one or a combination of bone nibblers or knife or soft tissue shaver (Dyonics 4.5 mm Synovator Blade; Forest Green, Smith & Nephew).
(A) Radial tubercle located through blunt dissection. (B) Digital palpation locating radial tuberosity.
In partial tears, the tendon is assessed with assistance of the speculum. In every case of a partial tear in this series, the remaining attached tendon was significantly tendinopathic. Therefore the remaining tendon attachment was carefully released from the tuberosity with a surgical blade to convert the injury to full thickness, prior to debriding the tuberosity and proceeding to repair using the aforementioned technique. For full thickness tears, the endoscope was not useful in preparation of the tuberosity.
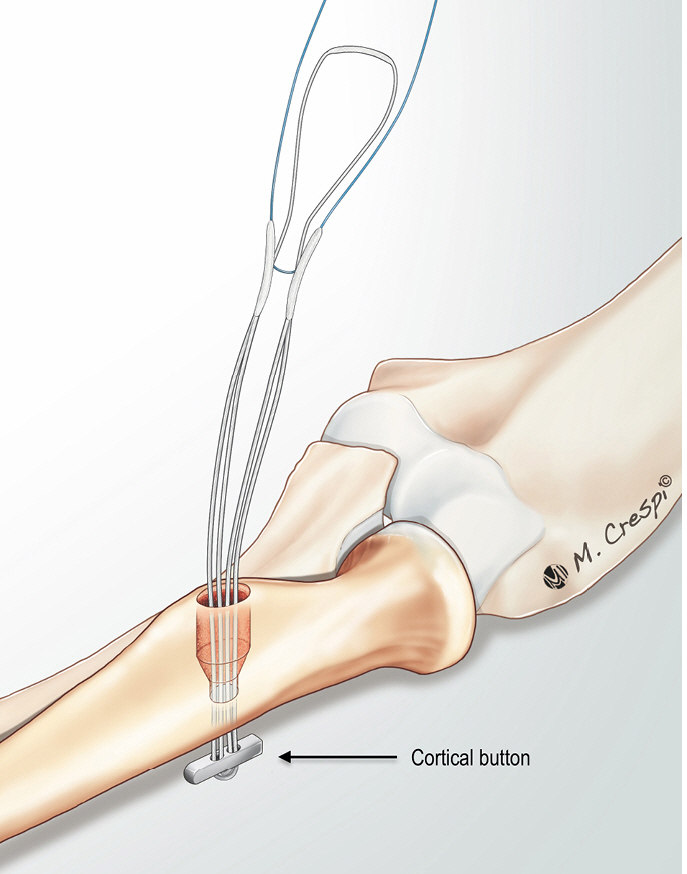
The bicipital tuberosity is prepared for tendon reattachment in a near anatomical manner using the Zimmer Biomet ToggleLoc system. The ZI-904754 Zimmer ToggleLoc with ZipLoop with a 13-mm button was used for repairs from 2011 until 2016. The construct was updated by the manufacturer and the ZI-110017308 ToggleLoc with needles and a 10.3-mm button was utilized from 2017 to 2021. The forearm is placed in maximum supination. The 2.9-mm drill is placed under direct vision, without the ToggleLoc translucent drill guide at this stage as it obscures vision of the drill entry point. The drill entry point is as far ulnar as possible on the tuberosity whilst allowing sufficient bone on the ulnar side to remain after the tendon tunnel is subsequently reamed. The drill is angled obliquely radially, and inserted until it is just through the far cortex. The drill guide can then be placed so as to protect the soft tissues during reaming. A 5-mm slotted reamer for average sized patients and a 6-mm one for larger patients is then used to create the tendon tunnel, preserving the far cortex (Fig. 4). The drill is removed leaving the reamer in place and a Zimmer Biomet ToggleLoc anchor is inserted through the slotted reamer. The reamer and drill guide are removed and the anchor sutures are gently pulled to ensure the anchor is well seated (Fig. 5). All bony debris are suctioned and the speculum is removed.
The proximal end of the tendon is typically in one of two locations. For virtually all partial tears and a minority of full thickness tears, the tendon is located within 2 cm of the tubercle and can be located using the speculum and a narrow Langenbeck retractor, without the endoscope being required. For most full thickness tears, the tendon end sits more proximally in the center of the arm approximately 2–4 cm above the elbow crease, and is often palpable externally. For tendon ends in this more proximal position, the surgeon’s finger can be used to make the initial passage to the tendon end and it is frequently possible for the surgeon to feel the end of the tendon with their fingertip. The hooded endoscope is inserted, with or without the speculum (Fig. 2) first placed along the tendon passage (Fig. 6). The hood of the endoscope is designed so that by angling it with the camera head pushed inferiorly, and the hooded tip tilted and directed superiorly, the hood is pushed upwards opening up the soft tissue window created by the endoscope, and speculum, if present.
When commencing this technique, there is a learning curve to identifying the position of the tendon end proximally. In patients within 1 to 2 weeks of injury of injury, the passage in which the tendon runs is typically still patent and the end of the tendon has not been walled-off or scarred; as the endoscope is gradually inserted, the tendon may appear in front of or superior to the tip of the endoscope. If the tendon end is not apparent, it may be located by withdrawing the endoscope partially to the elbow crease region and then reinserting in a more medial, lateral or superficial direction. The end of the tendon is often relatively superficial. At times the tendon end will have curled up onto itself. In more long-standing injuries, the tendon is harder to locate; using the endoscope, look for an area of whiter firm tissue in the areas described above; using blunt dissection with scissors, it can be determined if this represents the end of the tendon. Scissors are used to identify and tenolyse the end of the tendon to allow a clamp to be placed onto the tip. If required, a small additional incision can be made proximal to the elbow to locate the tendon end; however, with progressive experience at endoscopic tendon identification, the need for this second incision becomes rare.
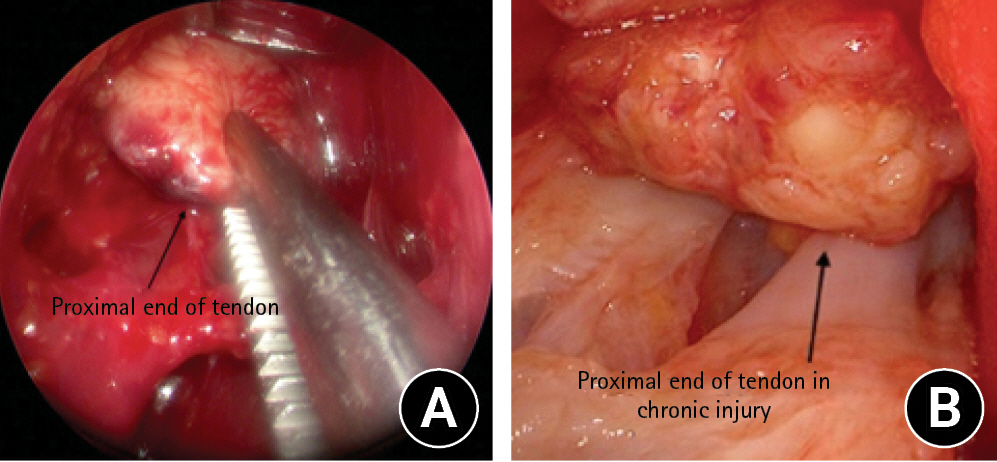
Once located, the tendon end is held with the tip of a long curved artery clamp or curved Kocher’s clamp. In acute injuries no tenolysis will be required (Fig. 7A), but in chronic cases (Fig. 7B) where the tendon end is scarred down, visualizing it with the endoscope and with an assistant holding the tendon under tension with the clamp, blunt dissection with scissors is used to free up the tendon. Once the tendon is sufficiently tenolysed, the elbow is flexed and the tendon end delivered out of the incision.
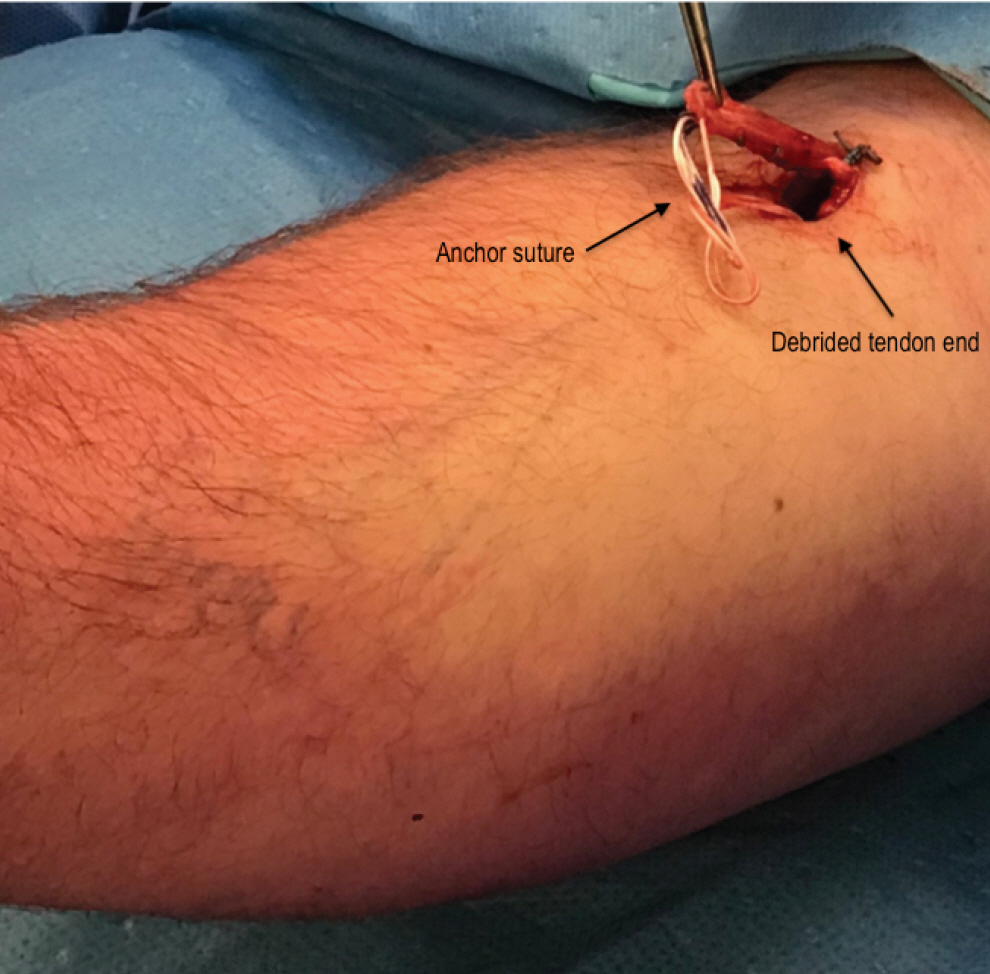
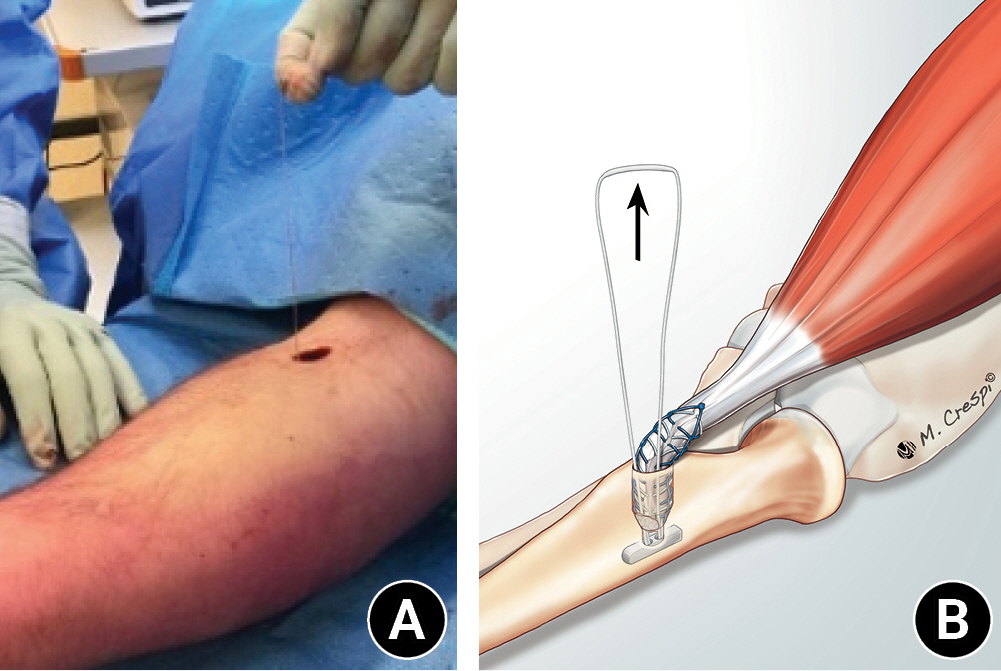
We would recommend first using this paper’s technique for acute full thickness retracted tears within 2 weeks of injury and progressing to more long-standing, less retracted tears and partial tears with experience. The tendon end requires preparation for repair. If the tendon end was originally unretracted it may not be possible to deliver the tendon externally; therefore, the debridement and repair is undertaken internally using the speculum and Langenbeck as retractors. The repair is easier when the tendon can be delivered externally. Tendinopathic tissue is debrided and a healthy tendon end created for repair. The tendon is sutured into the anchor with the suture using a locking whipstitch (Fig. 8). If the tendon is larger than the bony tunnel, the tunnel can be enlarged at this stage with a bony nibbler. The forearm is supinated and elbow flexed and the zip suture portion of the anchor is then pulled bringing the tendon end into the radial tuberosity tunnel (Fig. 9). The tendon repair is inspected and fluoroscopy can be used to ensure proper anchor placement. The wound is closed and a sling placed for comfort.
Rehabilitation
Patients were seen within 7 days of surgery by physical or occupational upper limb therapists. Education, wound care, and active and passive exercises were commenced, avoiding passive elbow extension. Hinged elbow splints were provided in 14.9% of cases (n=11/75) between 2011 and 2016, but in accordance with current evidence [23] were not used subsequent to this. Patients were advised on ultra-light use (<500 g) of the affected upper limb for activities of daily living for the first 6 weeks postoperation and cautioned against heavy use until 3 months. Light graded strengthening was commenced in the clinic from 6 weeks and patients were referred for gym-based rehabilitation towards 3 months if further reconditioning was required for their return to work or sport.
Statistical Analysis
Mean and standard deviation or range are provided for normally distributed data and median and interquartile range if skewed. The Fisher exact test was used to determine statistical differences in categorical variables between groups. Fisher’s exact test was chosen instead of the chi-square test to account for variables such as re-rupture, which had low numbers (<5). Α P-value of 0.05 was considered statistically significant.
RESULTS
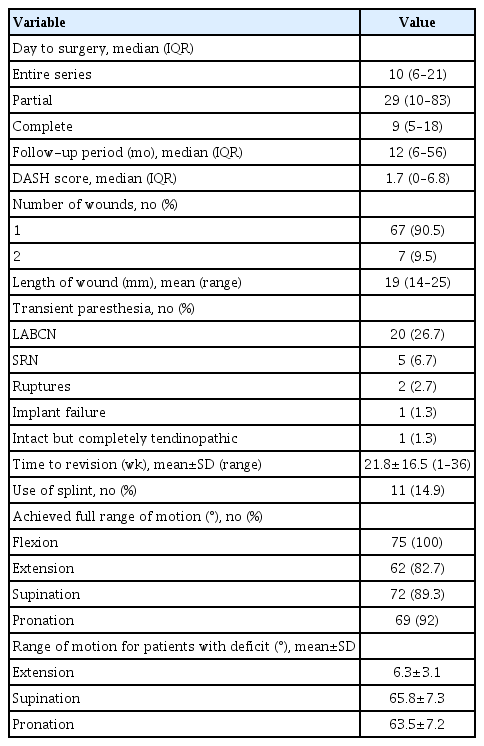
Median time from injury to surgery was 10 days (interquartile range [IQR], 6–21 days) for the entire series, with median 9 days (IQR, 5–18 days) for complete tears and 29 days (IQR, 10–83 days) for partial tears. Median time to follow-up was 12 months (IQR, 6–56 months). The median DASH score was 1.7/100 (IQR, 0–6.8). Sixty-seven of 74 patients (90.5%) had one wound, which was a mean 19 mm long (Table 2). A small area of transient paraesthesia was detected within the LABCN distribution in 26.7% (20/75) of cases, and in the superficial radial nerve in 6.7% (5/75) of cases, all of which resolved with expectant management within the follow-up time. There were no known symptomatic cases of heterotrophic ossification.
There was one case of implant failure which occurred 3 days following surgery. Surgical exploration revealed the point of failure to be the ToggleLoc loupe suture, with intact sutures within the tendon and good integrity of the tendon itself. The failure was reported to the manufacturer and the Australian Therapeutic Goods Administration.
There were two cases of re-rupture of the DBT. In both cases, re-rupture was preceded by significant shoulder or elbow pain. The first reported shoulder pain in the weeks following surgery but had an otherwise unremarkable recovery until onset of crepitus in the absence of new trauma at 6 months after repair. MRI investigation demonstrated retear of the DBT. The second case had previous ulnar nerve decompression undertaken at another center, and ulnar nerve transposition by the senior author 9 months prior to DBT repair. Recovery was complicated by persistent lateral elbow, upper arm and shoulder pain, which largely resolved within 9 weeks. Following this period the patient was not aware of any new trauma but noticed a change in muscle shape, with surgical exploration demonstrating failure of tendon healing. A further case underwent surgical exploration 8 months following initial repair due to continued elbow pain. Investigation revealed the tendon repair to be intact but highly tendinopathic and the tendinopathic tissue was excised and the repair revised.
Both cases of rupture and the case that underwent revision due to tendinopathy reported significant elbow or shoulder pain in the weeks preceding rupture or revision. There was a statistically significant difference (P=0.001) in the proportion of patients reporting significant pain between those who experienced re-rupture or required revision (n=3/3, 100%), compared with those who did not (n=6/71, 8.4%). There was no statistically significant difference in rupture rates between those who used splints and those who did not (P=0.28) and ruptures occurred past typical splinting periods. In the absence of noted traumatic events, the precise dates of re-rupture were unclear, but revisions occurred at 16 and 36 weeks after repair.
Full active flexion was achieved by all patients. Deficits in extension were observed in 13 patients (17.3%); of those with a deficit, mean extension was –6.3° (standard deviation [SD], 3.1°) A deficit in supination was observed in 8 cases (10.7%). Of these, mean supination was 65.8° (SD, 7.3°). Mean pronation in the 6/75 (8%) observed to have a deficit was 63.5° (SD, 7.2°).
DISCUSSION
This was a large single-center consecutive series of minimally invasive distal biceps repairs. This technique produced minimal morbidity and inconvenience during the recovery period. We considered several aspects of this technique to be particularly useful. Firstly, the use of a speculum as the sole retractor during preparation of the radial tuberosity and anchor placement provides excellent visualization of the key anatomical regions whilst minimizing soft tissue damage and risk of injury to neurovascular structures. Speculum use is not limited to any particular type of anchor. As the dissection to the radial tuberosity is limited to a relatively discrete tunnel, it is rare to have to diathermy or tie-off veins during this speculum approach, which results in less soft tissue disturbance and shorter surgical time. In addition, dissection within the forearm is undertaken bluntly, minimizing risk to the median nerve. The drill is stopped as soon as it passes through the far cortex of the radius and the anchor is placed using the attached guide, which situates the anchor just beyond the bone, reducing PIN injury risk. Finally, the hooded endoscope allows for retrieval and tenolysis of the avulsed tendon under direct vision. In each case of this series the tendon was repaired, including for partial tears, which all involved over 50% of the DBT, with the remaining attached tendon being tendinopathic. However, in the case lower grade partial tears with healthy remaining tendon, tendon debridement of the torn tendon could be considered with or without repair.
This paper documents repair using a cortical button placed through the far cortex and a tuberosity tunnel. The anchor was chosen because the ZipLoop of the anchor allows for easy prefabrication of the repair. However, other anchors or repair techniques could be incorporated into the endoscopic approach including those that avoid radial bone tunnels (thus reducing the risk of iatrogenic fracture) or extra-medullary anchors. Using intra-medullary metallic or all suture anchor devices for the repair would have the advantage of further reducing the risk of PIN injury. In chronic tears where the tendon is highly retracted, or in revision cases with highly tendinopathic tendon, tendon grafting of the biceps using palmaris longus, a hamstring tendon or other graft can be undertaken using the same incision, as typically the surgeon can deliver the tendon stump sufficiently from the incision to allow grafting of the tendon end.
The major complication occurring in this series was rupture of the tendon repair. The rupture rate was 2.7% (2/75), which is consistent with that reported in the literature for open cortical button repairs (2.9%) [24]. There were no cases of proximal radius fracture, vascular injury, or compartment syndrome in this study. Comparison with other data on minimally invasive DBT repairs is limited by a paucity of literature on this type of repair, and due to the relatively low number of cases in the published literature. Although a number of authors describe surgical techniques or cadaveric studies [10,22,25,26], few studies have reported patient outcomes of minimally invasive or endoscopically-assisted DBT repairs. Sharma and MacKay [19] described two endoscopic repairs using an Endobutton in 2005 and reported no complications for either case. Grégory et al. [9] reported on a cohort of 23 endoscopically-assisted repairs using a metallic suture anchor and reported 1 case (4.3% incidence) of PIN palsy on day 1 after surgery, which recovered within 3 weeks, and 1 case (4.3% incidence) of median nerve motor palsy and hypoesthesia attributed to hypertrophic scarring of the medial epicondyle aponeurosis. There were no re-ruptures and no cases of LABCN paresthesia reported. Bhatia described a single case of endoscopic repair of a retracted DBT using a three-portal technique and two suture anchors and reported no intra- or postoperative complications [21].
The most common adverse event was neuropraxia of the LABCN, which occurred in 26.7% cases (20/75), followed by superficial radial nerve neuropraxia in 6.6% cases (5/75). This was of no functional consequence, and all fully resolved, typically rapidly, through expectant management. A higher incidence of LABCN neuropraxia has typically been associated with open single incision approaches due to increased traction on the nerve via the use of retractors [27-29]. Grewal and colleagues compared single versus double-incision techniques and found a significantly higher rate with the single incision technique (19/47, 40.4%) compared with the double incision group (3/43, 7.0%) [30]. In their systematic review of clinical studies on open refixation techniques, Kodde et al. [28] report LABCN neuropraxia as the most common complication, with 66 of 764 cases (8.6%) lasting <6 months in the anterior incision group, compared with 14/310 (4.5%) in the two-incision group and 9/764 (1.2%) in the anterior group lasting >6 months. We believe the relatively high incidence of transient LABCN neuropraxia in our study is due to specific questioning of each patient regarding cutaneous sensory disturbance with a positive response recorded irrespective of severity. There were no cases of PIN, median nerve, or ulnar nerve palsy in our study. It is believed that the minimal soft tissue retraction permitted by use of the speculum reduces the risk of severe nerve damage.
The major strength of this study is a large number of patients treated consecutively with a uniform technique, often with a lengthy follow-up period. The major weakness is the retrospective nature of the study. Although all included cases were analyzed at least 6 months following surgery, follow-up times were variable. Isokinetic testing of supination strength was not available and we acknowledge that this is an important outcome measure following distal biceps repair. There was potential for measurement bias given range of motion outcomes were assessed in most cases with visual inspection as there were no observed deficits; however, all evaluations were completed by experienced and specialized staff. Anecdotally, we believe the severity of LABCN neuropraxia to be considerably less for minimally invasive procedures compared to our previous open operations.
CONCLUSIONS
In this series, minimally invasive DBT repair using a speculum and hooded endoscope produced satisfactory outcomes and led to minimal patient inconvenience during the recovery period, as indicated by low DASH scores. Major complications such as rupture were rare, and minor complications such as lateral cutaneous nerve paraesthesia resolved with expectant management.
Notes
Author contributions
Conceptualization: PJ. Formal analysis: ALB. Investigation: ALB. Investigation: PJ. Supervision: PJ. Writing-original draft: PJ, ALB. Writing-review & editing: PJ, ALB.
Conflict of interest
None.
Funding
None.
Data availability
Contact the corresponding author for data availability.
Acknowledgments
We would like to thank Emma Petta BSc (Nsg) for assistance in research design and data collection, and Jane Waddy BSc (Sports Science) MPhysio, Nicole Perera BSc (OT), and Simon Millichip B. Phys. Ed, Dip Physio, Post Grad Dip Physio. We are grateful to Dr Erin Cvejic BA (Hons) Psych PhD MBiostat GStat for assistance with statistical analysis.