|
 |
- Search
| Clin Shoulder Elb > Volume 26(3); 2023 > Article |
|
Abstract
Background
The purpose of this study was to identify demographics and risk factors associated with unplanned 30-day readmission and reoperation following open procedures for shoulder instability and examine recent trends in open shoulder instability procedures.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was queried using current procedural terminology (CPT) codes 23455, 23460, and 23462 to find patients who underwent shoulder instability surgery from 2015 to 2019. Independent sample Student t-tests and chi-square tests were used in univariate analyses to identify demographic, lifestyle, and perioperative variables related to 30-day readmission following repair for shoulder instability. Multivariate logistic regression modeling was subsequently performed.
Results
In total, 1,942 cases of open surgical procedures for shoulder instability were identified. Within our study sample, 1.27% of patients were readmitted within 30 days of surgery, and 0.85% required reoperation. Multivariate logistic regression modeling confirmed that the following patient variables were associated with a statistically significant increase in the odds of readmission: open anterior bone block/Latarjet-Bristow procedure, being a current smoker, and a long hospital stay (all P<0.05). Multivariate logistic regression modeling confirmed statistically significant increased odds of reoperation with an open anterior bone block or Latarjet-Bristow procedure (P<0.05).
Conclusions
Unplanned 30-day readmission and reoperation after open shoulder instability surgery is infrequent. Patients who are current smokers, have an open anterior bone block or Latarjet-Bristow procedure, or a longer than average hospital stay have higher odds of readmission than others. Patients who undergo an open anterior bone block or Latarjet-Bristow procedure have higher odds of reoperation than those who undergo an open soft-tissue procedure.
Shoulder instability has an estimated incidence of 23.9 per 100,000 individuals in the general population [1]. In traumatic settings, the incidence has been found to be even higher, affecting 1.7% of the general population [2]. Young patients have a higher risk of recurrent shoulder instability than older patients, predisposing them to recurrent dislocations, the development of Hill-Sachs defects, damage to the glenoid labrum, loss of glenoid bone stock, and early onset of glenohumeral osteoarthritis [3,4]. Management of these injuries is complex, with both operative and conservative options, and is based on patient goals, activity levels, and risk of recurrent shoulder instability. Prognostic factors for re-dislocation include younger age at the time of first dislocation, male sex, contact versus non-contact mechanisms, and degree of glenoid bone loss [2,5].
Multiple studies support the use of early operative stabilization over nonoperative management in preventing recurrent instability [6-8]. The most commonly performed procedures for recurrent shoulder instability are arthroscopic or open Bankart repair, the Latarjet-Bristow procedure, and an anterior bone block. Despite the success of arthroscopic Bankart repairs, the procedure is limited by a high risk of continued dislocation, which occurs in up to 20% of patients [4,9]. The optimal surgical treatment for patients with 15% to 20% of bone loss is unclear, with the Bankart repair and Latarjet-Bristow procedures demonstrating comparable results [3]. In patients with glenoid bone loss that exceeds 20%, the Latarjet-Bristow technique has traditionally been indicated and shown success, with studies reporting recurrent instability rates of only 4.7% at long-term follow-up [10]. Given the heterogeneity in management that exists, surgeons must account for the risk factors of readmission and reoperation when choosing a procedure. Previous studies have demonstrated that the open Latarjet-Bristow procedure has a higher risk of complications than an open Bankart repair, including the development of deep vein thromboembolism, surgical site infections, return to the operating room, and long operative times [11,12].
Although those complications are uncommon, the open Latarjet-Bristow procedure has historically been associated with higher perioperative and postoperative complications than open Bankart repairs. Few studies have examined the risk factors associated with unexpected readmission and reoperation following these procedures; therefore the purpose of this study was to identify the demographics and risk factors associated with the unplanned 30-day readmission and reoperation rate following open treatment for shoulder instability and examine the recent trend in these repair techniques. We hypothesized that the open Latarjet-Bristow technique would carry a higher risk of unexpected readmission and complications than the open Bankart procedure.
This study used the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. Trained clinical reviewers collected data from more than 700 participating hospitals, gathering patient demographics, comorbidities, surgery type in Current Procedural Terminology (CPT) codes, and 30-day postoperative surgical outcomes.
The ACS-NSQIP was queried using CPT codes 23455 ŌĆ£capsulorrhaphy, anterior; with labral repairŌĆØ (i.e., Bankart procedure), 23460 ŌĆ£capsulorrhaphy, anterior, any type; with bone block,ŌĆØ and 23462 ŌĆ£capsulorrhaphy, anterior, any type; with coracoid process transferŌĆØ (i.e., Latarjet-Bristow procedure) to find patients who underwent open surgery for shoulder instability from 2015 to 2019. The search yielded 1,942 cases. CPT code 23455 was compared against the combined total of CPT codes 23460 and 23462.
Data on the following demographic, lifestyle, and comorbidity variables were recorded: sex, age, body mass index (BMI), hypertension requiring medication, current tobacco use, diabetes mellitus, bleeding disorders, steroid use for a chronic condition, chronic obstructive pulmonary disease (COPD), American Society of Anesthesiologists (ASA) classification, and anesthesia technique. The primary outcome of 30-day readmission was defined as an unplanned hospital readmission likely related to the principal procedure. The secondary outcomes recorded were the presence of pneumonia, deep venous thrombosis (DVT)/thrombophlebitis, pulmonary embolism (PE), acute renal failure, bleeding requiring transfusion, systemic sepsis, wound complications (superficial surgical site infection or deep incisional surgical site infection), total operative time, hospital length of stay (if patient remained in the hospital for at least 1 day after surgery), discharge destination (home versus non-home), and reoperation.
All data were analyzed using the IBM SPSS ver. 23.0 (IBM Corp.). The criterion for statistical significance was set at ╬▒=0.05. Univariate analyses used chi-square and, where appropriate, FisherŌĆÖs exact tests to compare the open Bankart and open bone block/Latarjet-Bristow cohorts with regard to categorical demographic, comorbidity, lifestyle, and 30-day outcome variables. Student t-tests were used in a similar fashion for continuous outcome variables. Multiple logistic regression modeling was subsequently performed in a stepwise fashion to examine differences between the open Bankart and open bone block/Latarjet-Bristow cohorts while controlling for covariates. Descriptive statistics were used to complete a trend analysis comparing the two cohorts.
In total, 1,942 cases of open repair for shoulder instability were identified (open Bankart cohort: 1,167; open anterior bone block/Latarjet-Bristow cohort: 775). Demographic, lifestyle, and comorbidity profiles stratified by procedure type are presented in Table 1. In both cohorts, patients who underwent open Bankart repair for shoulder instability were significantly more likely to be ages 18 to 24, Žć2 (4, 1,942) = 23.83, P < 0.001, whereas patients who received an open anterior bone block/Latarjet-Bristow procedure were more likely to be 25 to 34, Žć2 (4, 1,942) = 23.83, P < 0.001. Patients from both cohorts were likely to be overweight: 41.7 vs. 40.8%, Žć2 (5, 1,921)=12.24, P=0.032. Patients in the open Bankart and open anterior bone block/Latarjet-Bristow cohorts were significantly likely to have an ASA classification of I and II, respectively: 48.2 vs. 52.1%, Žć2 (3, 1,942)=11.98, P=0.07. Patients in both cohorts typically received general instead of regional anesthesia: 96.0 vs. 97.8%, Žć2 (1, 1,937)=4.88, P=0.027. The two cohorts did not differ significantly in sex, hypertension, number of current smokers, or the incidence of diabetes mellitus, bleeding disorders, steroid use, or COPD.
The results of the univariate analyses comparing 30-day outcomes between the open Bankart and open anterior bone block/Latarjet-Bristow cohorts are displayed in Table 2. Patients who underwent an open anterior bone block/Latarjet-Bristow procedure were more likely to be readmitted than those who underwent open Bankart repair: 0.7 vs. 2.2%, Žć2 (1, 1,476)=6.53, P=0.016. Additionally, patients who underwent an open bone block/Latarjet-Bristow procedure typically had a longer mean operative time than the open Bankart cohort: 131.54┬▒53 vs. 99.13┬▒52.1 minutes, t(1,942)=27.60, P<0.001. Compared with patients who received an open Bankart repair, patients who underwent an open anterior bone block/Latarjet-Bristow procedure were significantly more likely to develop DVT/thrombophlebitis: 0.5 vs. 0.0%, Žć2 (1, 1,942)=6.04, P=0.025. Reoperation was also significantly more likely in the open anterior bone block/Latarjet-Bristow cohort than the Bankart cohort: 1.5 vs. 0.4%, Žć2 (1, 1,783)=6.46, P=0.016. The cohorts did not differ significantly in the presence of pneumonia, PE, acute renal failure, bleeding requiring transfusion, systemic sepsis, wound complications, hospital length of stay, or discharge destination. No patients died within 30 days of surgery.
The causes for reoperation and readmission in the two cohorts are identified in Table 3. Of the 1,942 patients included in our sample, only 1.27% were readmitted within the 30-day postoperative period. The results of the univariate analyses show statistically significant relationships between readmission status and the following patient variables (Table 4): being a current smoker, Žć2 (1, 1,476)=6.8, P=0.009, and hospital length of stay, 0.26┬▒0.8 vs. 1.21┬▒3.0 days, t(1,492)=6.32, P<0.001. Patient sex, age, BMI, ASA classification, anesthesia type, total operative time, and the presence of hypertension, diabetes mellitus, bleeding disorders, steroid use, and COPD were not associated with readmission.
Multivariate logistic regression modeling confirmed that the following patient variables were associated with significantly increased odds of readmission (Table 5): open bone block/Latarjet-Bristow procedure (P=0.018; odds ratio [OR], 3.34; 95% confidence interval [CI], 1.23ŌĆō9.09); current smoker (P=0.012; OR, 3.34; 95% CI, 1.30ŌĆō8.57); and hospital length of stay (P<0.001; OR, 1.39; 95% CI, 1.12ŌĆō1.66).
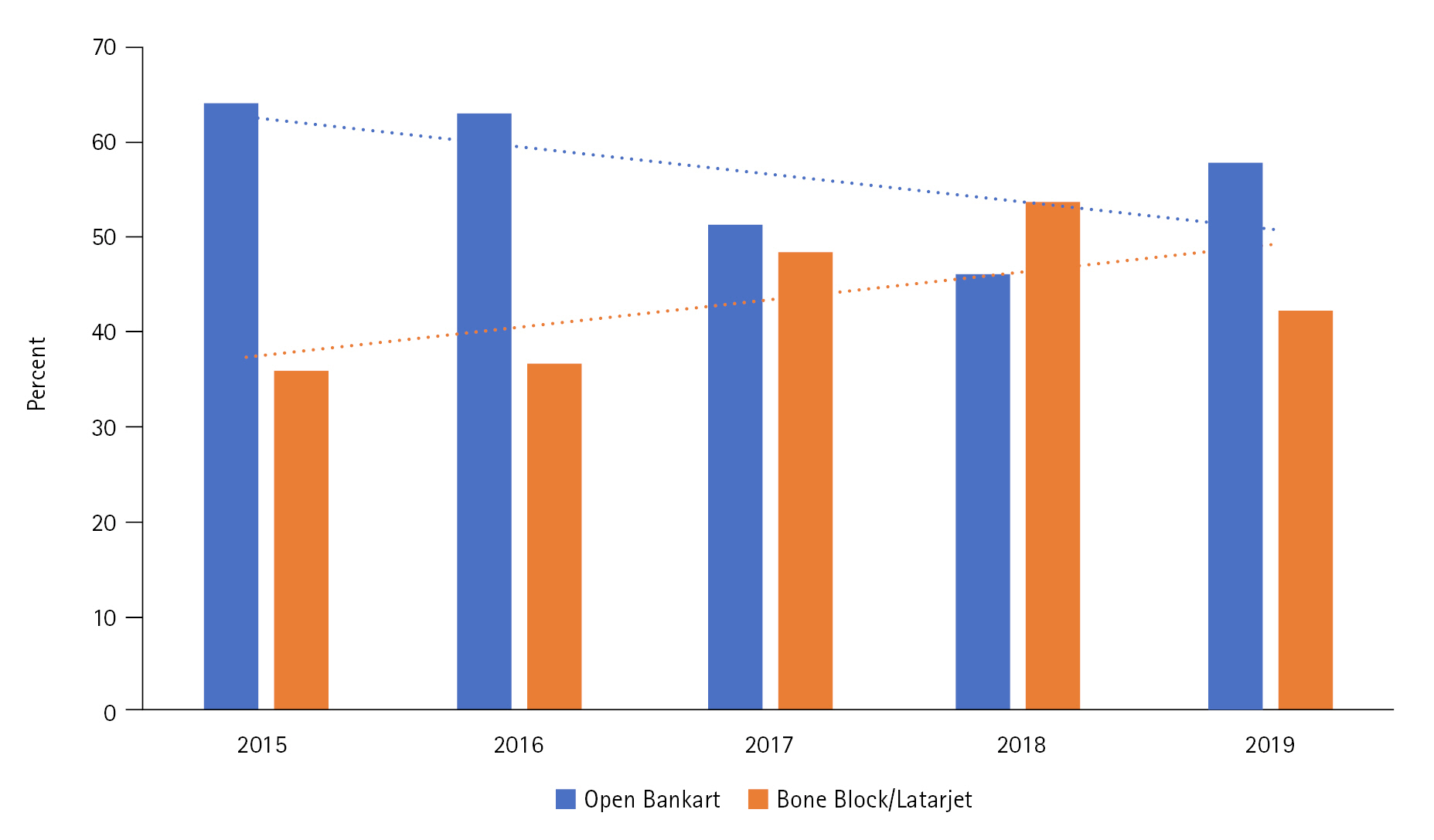
Of the 1,942 patients included in our sample, only 0.85% underwent reoperation within the 30-day postoperative period. The univariate analysis did not reveal any statistically significant relationships between reoperation and patient variables (all P>0.05). Multivariate logistic regression modeling confirmed that only procedure type, open bone block/Latarjet-Bristow procedure, was associated with a statistically significant increase in the odds of reoperation (P=0.019; OR, 3.98; 95% CI, 1.26ŌĆō12.53). Our 5-year trend analysis demonstrates a significant increase in the number of bone block and Latarjet-Bristow procedures and a decline in open Bankart repairs from 2015 to 2019 (r=0.61, P<0.001) (Fig. 1).
To assist in clinical decision making, we have here identified recent trends, demographics, and risk factors for readmission associated with open repair of shoulder instability (the Bankart, anterior bone block, and Latarjet-Bristow techniques). Our study expands on the previously published literature to provide a more complete understanding of the perioperative and postoperative risks associated with open shoulder stabilization. Consistent with previous studies, the open Latarjet-Bristow procedure was found to be associated with a statistically significant increase in the risk of developing DVT, reoperation, and readmission, compared with the open Bankart procedure. Additionally, the open Latarjet-Bristow technique was associated with longer total operative times, potentially contributing to the increased risk for perioperative and postoperative complications. Of additional clinical relevance, we identified three independent risk factors for readmission and one independent risk factor for reoperation following the open management of shoulder instability. The risk factors for readmission are current smoking status, length of hospital stay, and procedure performed (anterior bone block or Latarjet-Bristow compared with open Bankart). The Latarjet-Bristow procedure and anterior bone blocks also had higher odds for reoperation. This retrospective review of shoulder instability patients could enable risk stratification, patient education, and informed clinical decision making, especially for patients with subcritical glenoid bone loss.
Proper identification and management of shoulder instability is important due to the risk of developing labral damage, osseus defects causing recurrent instability, and early-onset glenohumeral arthritis [3,4]. An important determinant in the management of recurrent instability is the amount of glenoid bone stock, with increased bone loss associated with recurrent instability due to alterations in the static restraint function of the shoulder [2]. Although the literature varies in defining how much bone loss is critical, the general consensus is that glenoid bone loss of less than 15% should be treated with Bankart procedures (open or arthroscopic), and those with more than 20% of bone loss are best treated with the Latarjet-Bristow technique [1,4,11,13]. Both open Bankart and open Latarjet-Bristow procedures are performed for patients with intermediate glenoid bone loss (15%ŌĆō20%), so clinical decision-making must include an understanding of the safety and long-term success of each treatment option. Although previous studies have found the Latarjet-Bristow technique to be associated with a lower risk of recurrent dislocation and better patient-reported outcomes than the Bankart procedure, the Latarjet-Bristow procedure is also associated with an increased risk of complications, such as superficial infections, superficial and deep vein thrombosis, return to the operating room, and musculocutaneous neuropraxia [11,12].
Our study demonstrates that the open Latarjet-Bristow and open bone block procedures are associated with a significantly higher incidence of reoperation and readmission than the open Bankart repair (3.1% vs. 0.86%) at 30-day follow up. This is consistent with previous literature demonstrating complication rates for the Latarjet-Bristow procedure ranging from 1.9% to 5.5%ŌĆöwhich is 8 to 9 times higher than that reported for Bankart repairs [12]. Additionally, the Latarjet-Bristow technique was associated with an increased risk of developing DVT 30-day postoperative period, which supports prior studies that found an approximate five-times increase in the risk in thromboembolic complications in open Latarjet-Bristow versus Bankart repair [12].
Regarding operative time, our data confirm that the Latarjet-Bristow technique and anterior bone blocks are associated with longer operative periods than open Bankart repairs. Although prolonged surgical times have been associated with an increased risk of surgical site infections, we did not find a significant difference in superficial or deep surgical site infections between the groups [14]. Nonetheless, recent literature has found the open Latarjet-Bristow technique to have higher rates of deep surgical site infection than the Bankart method [12,14].
When comparing risk factors for readmission following the open management of shoulder instability, we identified three statistically significant risk factors associated with readmission in the 30-day postoperative period: smoking, procedure type, and length of hospital stay following the initial operation. For procedure type, we found that the open Latarjet-Bristow technique and open bone block procedures were a significant risk factor for readmission (OR, 3.34), whereas the open Bankart procedure was not. The most common causes for readmission in those who underwent open Latarjet-Bristow or open bone block procedures were wound disruption (30.8%), DVT (7.7%), and sepsis (7.7%). The only risk factor found to predict reoperation was the type of procedure performed, with the open Latarjet-Bristow and bone block procedures being more likely to require reoperation than an open Bankart procedure (OR, 3.98). The reasons for reoperation included incision and drainage for hematoma or infection and revision of the bone block procedure.
This study is not without limitations. To identify patients in the NSQIP database, CPT codes were queried, so miscoding might have led to incomplete patient capture. The database is reported by participating hospitals and thus might not be generalizable to all patient populations, particularly those in free-standing ambulatory surgery centers. In addition, postoperative data were collected for only 30 days. Complications, including those evaluated in this study (DVT, PE, infections, reoperation, and readmission) often occur outside of the 30-day period. Nonetheless, the NSQIP database has been used to evaluate complication and readmission rates associated with many other orthopedic procedures [11,14-18].
Our study is consistent with previous literature that found that the open Latarjet-Bristow technique is associated with a slightly increased risk of readmission and reoperation compared with the open Bankart procedure. Additionally, we determined that current smokers and those with prolonged hospital stays after the index procedure have the highest risk of reoperation and/or readmission following any open surgery for shoulder instability (Bankart, anterior bone block, or Latarjet-Bristow). To our knowledge, this is the largest study to make a matched-cohort comparison of open treatments for shoulder instability. Early identification and management of patients with shoulder instability is critical to achieving successful long-term outcomes and improving patient satisfaction. This retrospective review of shoulder instability patients could be useful for risk stratification, patient education, and informed clinical decision making, especially for patients with subcritical glenoid bone loss.
NOTES
Author contributions
Conceptualization: JMT, MJP, RMC. Data curation: JMT. Formal analysis: JMT. Investigation: JMT. Methodology: JMT. Project administration: JMT. Resources: JMT. Software: JMT. Supervision: JMT, MJP, RMC. Validation: JMT. Visualization: JMT, RMC. Writing-original draft: JMT, AD. Writing-review & editing: JMT, MJP, BK, LB, RMC.
Fig.┬Ā1.
Percentage of open Bankart versus anterior bone block and Latarjet-Bristow procedures from 2015 to 2019.
Table┬Ā1.
Demographics and comorbidities between open Bankart and open bone block/Latarjet-Bristow procedures
| Variable | Open Bankart cohort | Open anterior bone block/Latarjet-Bristow cohort | P-value |
|---|---|---|---|
| Case | 1,167 (60.1) | 775 (39.9) | |
| Sex | 0.076 | ||
| ŌĆāMale | 958 (82.1) | 660 (85.2) | |
| ŌĆāFemale | 209 (17.9) | 115 (14.8) | |
| Age (yr) | <0.001* | ||
| ŌĆā<18 | 1 (0.1) | 0 | |
| ŌĆā18ŌĆō24 | 443 (38.0) | 284 (36.6) | |
| ŌĆā25ŌĆō34 | 373 (32.0) | 317 (40.9) | |
| ŌĆā35ŌĆō44 | 190 (16.3) | 108 (13.9) | |
| ŌĆāŌēź45 | 160 (13.7) | 66 (8.5) | |
| Body mass index (kg/m2) | 0.032* | ||
| ŌĆāUnderweight | 4 (0.3) | 9 (1.2) | |
| ŌĆāNormal weight | 365 (31.7) | 266 (34.6) | |
| ŌĆāOverweight | 481 (41.7) | 313 (40.8) | |
| ŌĆāObese, class I | 200 (17.3) | 133 (17.3) | |
| ŌĆāObese, class II | 63 (5.5) | 34 (4.4) | |
| ŌĆāObese, class III | 40 (3.5) | 13 (1.7) | |
| Comorbidity | |||
| ŌĆāHypertension | 89 (7.6) | 62 (8.0) | 0.763 |
| ŌĆāCurrent smoker | 285 (24.4) | 220 (28.4) | 0.051 |
| ŌĆāDiabetes | 24 (2.1) | 8 (1.0) | 0.082 |
| ŌĆāBleeding disorders | 0 | 2 (0.3) | 0.189 |
| ŌĆāSteroid use | 7 (0.6) | 3 (0.4) | 0.749 |
| ŌĆāChronic obstructive pulmonary disease | 6 (0.5) | 2 (0.3) | 0.489 |
| ASA classification | 0.007* | ||
| ŌĆāClass I | 562 (48.2) | 319 (41.2) | |
| ŌĆāClass II | 515 (44.1) | 404 (52.1) | |
| ŌĆāClass III | 88 (7.5) | 51 (6.6) | |
| ŌĆāClass IV | 2 (66.7) | 1 (33.3) | |
| Anesthesia technique | 0.027* | ||
| ŌĆāGeneral | 1,118 (96.0) | 755 (97.8) | |
| ŌĆāRegional | 47 (4.0) | 17 (2.2) |
Table┬Ā2.
Univariate analysis of 30-day outcomes between open Bankart and open bone block/Latarjet-Bristow procedures
Table┬Ā3.
Causes of readmission and reoperation
Table┬Ā4.
Demographic, lifestyle, comorbidity, and perioperative factors and readmission following open Bankart and open anterior bone block/Latarjet-Bristow procedures
REFERENCES
1. Shields DW, Jefferies JG, Brooksbank AJ, Millar N, Jenkins PJ. Epidemiology of glenohumeral dislocation and subsequent instability in an urban population. J Shoulder Elbow Surg 2018;27:189ŌĆō95.


2. Rosa JR, Checchia CS, Miyazaki AN. Traumatic anterior instability of the shoulder. Rev Bras Ortop 2017;52:513ŌĆō20.



3. Galvin JW, Ernat JJ, Waterman BR, Stadecker MJ, Parada SA. The epidemiology and natural history of anterior shoulder instability. Curr Rev Musculoskelet Med 2017;10:411ŌĆō24.



4. Provencher MT, Bhatia S, Ghodadra NS, et al. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am 2010;92 Suppl 2:133ŌĆō51.


5. Wasserstein DN, Sheth U, Colbenson K, et al. The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy 2016;32:2616ŌĆō25.


6. Arciero RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med 1994;22:589ŌĆō94.


7. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med 2002;30:576ŌĆō80.


8. Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy 1989;5:213ŌĆō7.


9. Dora C, Gerber C. Shoulder function after arthroscopic anterior stabilization of the glenohumeral joint using an absorbable tac. J Shoulder Elbow Surg 2000;9:294ŌĆō8.


10. Schroder DT, Provencher MT, Mologne TS, Muldoon MP, Cox JS. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen. Am J Sports Med 2006;34:778ŌĆō86.


11. Bokshan SL, DeFroda SF, Owens BD. Comparison of 30-day morbidity and mortality after arthroscopic bankart, open bankart, and latarjet-bristow procedures: a review of 2864 cases. Orthop J Sports Med 2017;5:2325967117713163.



12. Goodloe JB, Traven SA, Johnson CA, Woolf SK, Nutting JT, Slone HS. Increased risk of short-term complications and venous thromboembolism in Latarjet-Bristow procedures compared with bankart repairs. Arthroscopy 2021;37:806ŌĆō13.


13. Olds MK, Ellis R, Parmar P, Kersten P. Who will redislocate his/her shoulder? Predicting recurrent instability following a first traumatic anterior shoulder dislocation. BMJ Open Sport Exerc Med 2019;5:e000447



14. Eberlin CT, Varady NH, Kucharik MP, Naessig SA, Best MJ, Martin SD. Comparison of perioperative complications following surgical treatment of shoulder instability. JSES Int 2022;6:355ŌĆō61.



15. Martin CT, Gao Y, Pugely AJ, Wolf BR. 30-Day morbidity and mortality after elective shoulder arthroscopy: a review of 9410 cases. J Shoulder Elbow Surg 2013;22:1667ŌĆō75.


16. Martin CT, Pugely AJ, Gao Y, Wolf BR. Risk factors for thirty-day morbidity and mortality following knee arthroscopy: a review of 12,271 patients from the national surgical quality improvement program database. J Bone Joint Surg Am 2013;95:e98.