|
 |
- Search
| Clin Shoulder Elb > Volume 25(4); 2022 > Article |
|
Abstract
Background
Chronic subscapularis tendon tear (SBT) is a degenerative disease and a common pathologic cause of shoulder pain. Several potential risk factors for chronic SBT have been reported. Although metabolic abnormalities are common risk factors for degenerative disease, their potential etiological roles in chronic SBT remains unclear. The purpose of this study was to investigate potential risk factors for chronic SBT, with particular attention to metabolic factors.
Methods
This study evaluated single shoulders of 939 rural residents. Each subject undertook a questionnaire, physical examinations, blood tests, and simple radiographs and magnetic resonance imaging (MRI) evaluations of bilateral shoulders. Subscapularis tendon integrity was determined by MRI findings based on the thickness of the involved tendons. The association strengths of demographic, physical, social, and radiologic factors, comorbidities, severity of rotator cuff tear (RCT), and serologic parameters for SBT were evaluated using logistic regression analyses. The significance of those analyses was set at p<0.05.
Results
The prevalence of SBT was 32.2% (302/939). The prevalence of partial- and full-thickness tears was 23.5% (221/939) and 8.6% (81/939), respectively. The prevalence of isolated SBT was 20.2% (190/939), SBT combined with supraspinatus or infraspinatus tendon tear was 11.9% (112/939). In multivariable logistic regression analysis, dominant side involvement (p<0.001), manual labor (p=0.002), diabetes (p<0.001), metabolic syndrome (p<0.001), retraction degree of Patte tendon (p<0.001), posterosuperior RCT (p=0.010), and biceps tendon injury (p<0.001) were significantly associated with SBT.
The function of the subscapularis muscle and the integrity of the subscapularis tendon are of great importance to shoulder function. Providing approximately 50% of rotator cuff force, the subscapularis is the largest and most powerful of the rotator cuff muscles and its importance in arm elevation outweighs that of both the supraspinatus and infraspinatus [1,2]. Since 1934, when Codman stated that the subscapularis accounted for merely 3.5% of 200 rotator cuff tears (RCTs), the prevalence of subscapularis tendon tear (SBT) has been considered to be much lower than that of supraspinatus tendon tear [3]. An magnetic resonance imaging (MRI) study of 2,167 patients with RCTs revealed a low prevalence of SBT at 2%, of which partial and full-thickness tears accounted for 27% and 73%, respectively [4]. In contrast, several reports have shown the prevalence of SBT to be as high as 30% in all arthroscopic shoulder surgeries and up to 49.4% in arthroscopic rotator cuff procedures [5-7]. To the best of our knowledge, there are no available reports regarding SBT prevalence in non-hospitalized populations.
Chronic SBT is a common pathologic cause of shoulder pain. However, the etiology of chronic SBT remains incompletely understood. Several previous studies that focused mostly on anatomical or radiological parameters have investigated potential SBT risk factors, including subcoracoid stenosis [8], coracoid process morphology (coracoid angle and coracoid distal length) and greater humeral version [9], coracohumeral distance and coracoid overlap [10,11], subscapularis tendon slip number [11], lesser tuberosity cyst [12], coracohumeral index and coracoglenoid inclination [13], and the size of posterosuperior RCT (PSRCT) and long head of biceps tendon (LHBT) tear [14]. Several metabolic abnormalities or factors, including diabetes or hyperglycemia, dyslipidemia, and metabolic syndrome, have been reported as risk factors for tendinopathy. However, studies investigating the specific association of chronic SBT with metabolic factors, which are known risk factors for degenerative diseases, are lacking. We hypothesized that metabolic factors are associated with chronic SBT; therefore, the purpose of this study was to investigate potential risk factors for chronic SBT, with particular attention to metabolic factors.
This study was approved by the Institutional Review Board of Gyeongsang National University Hospital (No. GNUH 2015-02-001). Informed consent was obtained from the volunteers included in this study.
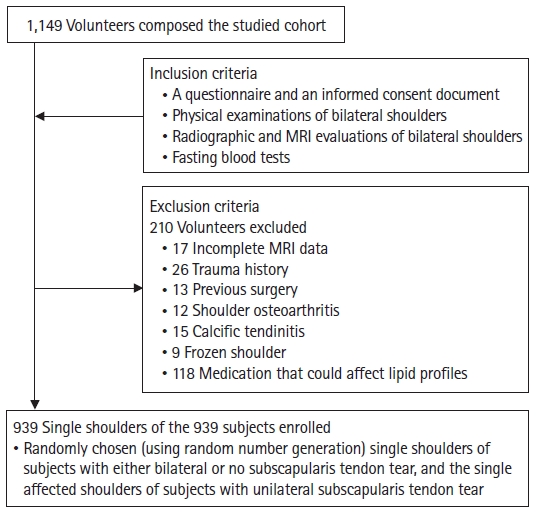
A survey of upper extremity morbidity was conducted with support from public health officers. The study cohort was comprised of 1,149 uncompensated volunteers from the studied rural region. One of those recruited volunteers had an amputated shoulder; therefore, 2,297 shoulders were included in the study cohort. Of these volunteers, study subjects were enrolled according to the following inclusion and exclusion criteria. The inclusion criteria were the completion of a written consent and of a questionnaire, physical examinations, fasting blood tests, and simple radiographs (true anteroposterior, axillary lateral, and outlet views) and MRI evaluations of bilateral shoulders. The exclusion criteria were a lack of participation in shoulder MRI studies (n=17), a relevant history of trauma (n=26), previous shoulder surgery (n=13), glenohumeral joint osteoarthritis (n=12), calcific tendinitis (n=15), frozen shoulder (n=9), and/or use of medications that could affect serum lipid profiles (n=118). After exclusion, a total of 939 enrolled subjects, of whom 462 were male and 477 were female with a mean age of 59.2┬▒8.4 years, were included in the study. Because several non-systemic variables are shoulder-related factors that would not affect both bilateral shoulders similarly, only one shoulder per subject was included in the analysis as the studied side to evaluate the strength of associations among variables. For subjects with either bilateral SBT or no SBT, one shoulder was randomly included (using random number generation by Excel). For each subject with unilateral SBT, only the involved shoulder was included as the studied side (Fig. 1).
MRIs were performed using a 1.5-T scanner (Siemens Medical Systems, Erlangen, Germany). Four sequences, each with a slice thickness of 3 mm, a field of view from 15.9 to 18.0 cm, and one excitation, were obtained as follows: (1) oblique sagittal T1-weighted spin echo, (2) oblique sagittal T2-weighted turbo-spin-echo (TSE) with fat saturation, (3) oblique coronal T2-weighted TSE with fat saturation, and (4) axial T2-weighted TSE with fat saturation. All MRIs were interpreted by one experienced musculoskeletal radiologist who was blind to the clinical findings (JBN). Full thickness RCTs were diagnosed based on a discontinuity or gap in the tendon or an increased signal intensity on T2-weighted images, extending from the articular to the bursal surfaces. Partial thickness RCTs were diagnosed based on partial high intensity in the rotator cuff tendon or on a slight increase in signal intensity in the cuff tendon, without a definite defect on either the intra-articular or the bursal side. Biceps tendon injuries were determined by MRI, then classified as partial or complete tear, or subluxation. Partial biceps tendon tear was identified by increased intra-tendinous T2-weighted signal intensity. A complete tear was identified by absence of the LHBT intra-articularly or within the bicipital groove. Subluxation was identified by displacement of the LHBT from the bicipital groove [15].
The studied variables were as follows. The demographic or general physical factors included age, sex, waist circumference, and dominant side involvement. The social factors included tobacco smoking, alcohol use, and manual labor and the comorbidities included diabetes, hypertension, metabolic syndrome, and dyslipidemia. Previous diagnoses of diabetes and hypertension were accepted. New diagnoses were made during the study using current standards for blood test and blood pressure findings as follows: diabetes, by serum levels of glycated hemoglobin (HbA1c) Ōēź6.5% or of fasting glucose Ōēź126 mg/dL [16] and hypertension, by blood pressure >140 mmHg in systolic or >90 mmHg in diastolic [17]. Clinical identification of metabolic syndrome involved meeting at least three of these five criteria: (1) fasting plasma glucose level Ōēź100 mg/dL or use of antidiabetic medication, (2) systolic blood pressure Ōēź130 mmHg or diastolic blood pressure Ōēź85 mmHg, or use of antihypertensive medication, (3) serum triglyceride (TG) level Ōēź150 mg/dL, (4) serum high-density lipoprotein (HDL) level <40 mg/dL for men or <50 mg/dL for women, and (5) waist circumference Ōēź90 cm for men or Ōēź85 cm for women [18,19]. The serological factors were cholesterol, TG, low-density lipoprotein (LDL), HDL, non-HDL (non-HDL), and TG/HDL Ōēź3.5. Dyslipidemia was determined, using these criteria: hypercholesterolemia (total cholesterol Ōēź200 mg/dL), hyper-LDLemia (LDL Ōēź100 mg/dL), hyper-TGmia (TG Ōēź150 mg/dL), hypo-HDLemia (HDL <40 mg/dL for men and <50 mg/dL for women), and hyper-non-HDLemia (non-HDL Ōēź130 mg/dL) [20].
Factors related to tear chronicity detected on MRI were Patte retraction degree [21], global fatty degeneration index [22], Goutallier grade of infraspinatus [23], tangent sign [24], and occupation ratio [25]. The radiographic factor was superior displacement of the humeral head [26]. The factors related to tendon involvement were posterosuperior cuff tear and biceps tendon injury. These factors and their prevalence are summarized in Table 1.
The prevalence and 95% confidence intervals (CIs) of SBTs were analyzed. Using univariate logistic regression analyses, the odds ratios and 95% CIs were calculated to identify any association between SBT and the studied variables. Then, multivariable logistic regression analyses, using only the significant variables identified in the univariate analyses, were performed. Multivariable logistic regression analysis was performed after assessment of multicollinearity using factors with both a variance inflation factor and a condition index <10, indicating no multicollinearity [27]. The goodness of fit for a multivariable logistic regression model was determined using the Hosmer-Lemeshow test. All statistical analyses were performed using the IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA). The significance of the logistic regression analyses and the Hosmer-Lemeshow test were set at p<0.05.
The prevalence of SBT among enrolled subjects was 32.2% (302/939); among subjects with overall RCT, it was 74.6% (302/405). The prevalence of SBT when isolated, when combined with PSRCT, and in relation to tear thicknesses is summarized in Table 2. In univariate analyses, age, male sex, dominant side involvement, manual labor, diabetes, metabolic syndrome, TG/HDL Ōēź3.5, Patte retraction degree, global fatty degeneration index, Goutallier grade, occupation ratio, PSRCT, and biceps tendon injury were significantly associated with SBT (pŌēż0.006) (Table 3).
In multivariable analysis, dominant side involvement, manual labor, diabetes, metabolic syndrome, Patte retraction degree, PSRCT, and biceps tendon injury were significantly associated with SBT (pŌēż0.041) (Table 4). The p-value of the Hosmer-Lemeshow test was 0.427, indicating a good fit.
A notable finding of this study is that metabolic syndrome is a significantly associated factor for SBT, as are the following previously-reported significantly associated factors: dominant side involvement, manual labor, diabetes, Patte retraction degree, PSRCT, and biceps tendon injury. Metabolic syndrome is a well-known risk factor for various degenerative diseases, among which are cardiovascular disease, stroke, diabetes, osteoarthritis, and Achilles enthesopathy [28-30]. Metabolic syndrome has also been reported as significantly associated with PSRCT [31]. The current study found, by multivariable analysis and after adjustment for the PSRCT variable, that metabolic syndrome is an independently associated factor for chronic SBT. This finding suggests that the degenerative effect of metabolic syndrome, evident on PSRCT and other tendon tears, also heightens the risk of SBT [30,31]. This finding strongly suggests that metabolic syndrome is a risk factor for SBT. The molecular mechanism and the pathophysiology of that association have not been determined; therefore, future research is needed to clarify the underlying molecular mechanisms and the effect of metabolic syndrome on subscapularis tendon degeneration or tendinopathy.
The prevalence of SBT was found by one cadaveric study to be 37% and also found that all tears were articular side partial tears [32]. According to studies based on arthroscopic findings, the prevalence of SBT was from 27% to 49.4% in all shoulder arthroscopy recipients [5,7]. Several previous studies have reported that SBT was frequently associated with PSRCT [33,34]. One study reported that intra-articular partial SBT was detected in 19% of patients who had arthroscopy and that SBT was significantly associated with supraspinatus and infraspinatus tendon tears [35]. One MRI study of patients visiting a hospital reported about 80% of the SBTs as being combined with PSRCT [4]. In the current study, SBT was significantly associated with PSRCT; the prevalence of SBT in overall RCT was 74.6%. The current study confirmed previous findings that SBT is frequently associated with PSRCT.
The current study found dominant-side involvement to be a significantly associated factor of SBT. Most previous relevant studies reported the greater prevalence of RCT on the dominant side [31,36]. No relation between hand dominance and SBT was found by Mehta et al. [37]; however, the study design differed from that of the present study by including asymptomatic SBT patients. In the present study, which included subjects with either symptomatic or asymptomatic SBT, the involvement of the dominant side was identified as a risk factor for SBT, similar to its role in PSRCT [31]. In addition, manual labor was significantly associated with SBT in the present study. Previous epidemiologic studies indicated high prevalence of RCT among manual laborers, including agricultural workers. Some previous biomechanical studies suggested that manual labor activities, including sustained or repeated arm abduction, heavy lifting or carrying, high task repetitiveness, and physical exertion, are associated with PSRCT [38]. Findings in this study suggest that repetitive manual activity or overuse are a common cause of tendon degeneration and are involved in the development of SBT, similarly as in PSRCT.
The main finding of this study that diabetes is strongly associated with SBT is consistent with the findings of several previous studies that noted diabetes as a risk factor for RCT and for retear after rotator cuff repair [39,40]. One previous study reported a significant association between hyperglycemia and Achilles tendon tendinopathy and found insulin resistance, an aspect of metabolic syndrome, to be a risk factor for tendinopathy [41]. According to another report, even plasma glucose levels at the high end of the normal range may be a risk factor for RCT [42]. On the molecular level, hyperglycemia induces oxidative stress and cytokine production, which lead to inflammation and result in damage to various tissues [43]. Hyperglycemia alters collagen structure through a glycation process, and it also reduces proteoglycan levels through decreased synthesis or sulfation of glycosaminoglycans [44,45]. These molecular mechanisms may affect tendon degeneration, including SBT. Results of the current study are consistent with and support the findings of previous studies regarding the association of diabetes with tendinopathy or tendon tear.
In this study, Patte retraction degree was significantly associated with SBT. The retraction degree has been reported to be significantly associated with supraspinatus muscle atrophy, which could explain the tear severity and/or tear chronicity of supraspinatus tear that is associated with SBT [46]. Mehta et al. [37] reported that SBT and LHBT pathology are significantly related to the size of the PSRCT. The results from this study confirm those of previous studies and they support the finding that chronic PSRCT is a potential risk factor for SBT.
Several studies reported that lesions of the LHBT are significantly associated with SBT [7,32,47]. Chen et al. [48] reported that 97% of RCTs with subscapularis tendon involvement are combined with LHBT lesions. Several MR studies have reported that medial subluxation or dislocation of the LHBT is associated with SBT [47,49]. Hidden biceps tendon instability has also been reported as a factor associated with SBT [50]. One study reported a sentinel sign, in which biceps tendon scuffing, abrasion, or partial tear of the anterior portion can serve as a warning to clinicians about the presence of SBT [51]. The present study confirms the results of previous studies that found that SBT is significantly associated with biceps long head lesions.
This cross-sectional study has some limitations. Subjects included volunteers only, and they may not have been representative of the entire local population. Agricultural workers made up a major portion of this cohort, and their characteristics may not be generalizable to other populations in other locations. This study did not evaluate differences in ethnic backgrounds, family histories, educational attainments, or activity levels. SBT and biceps tendon injury were diagnosed by 1.5-T MRI, which has been reported to have less diagnostic accuracy than arthroscopy or 3.0-T MRI [14,52]. To minimize the compound variable effect, subjects being medicated with any lipid-lowering drug were excluded, which might affect the study results through reduction of the sample size. However, because supplemental analyses conducted without that exclusion yielded similar results, the exclusion potential for bias is likely to be small and acceptable (Supplementary Table 1). Metabolic syndrome is a potential risk factor for SBT, as are these factors: overuse, diabetes, PSRCT, increased retraction of posterosuperior rotator cuff tendon, and biceps tendon injury.
NOTES
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.5397/cise.2021.00710.
Fig.┬Ā1.
Flowchart for inclusion and exclusion criteria for this study. All 939 subjects met the authorsŌĆÖ inclusion and exclusion criteria. MRI: magnetic resonance imaging.
Table┬Ā1.
The summary of demographic data, prevalence, mean or median for each of studied variables
Table┬Ā2.
Prevalences of SBT among enrolled subjects
Table┬Ā3.
Factors significantly associated with subscapularis tendon tear in univariate analyses
Table┬Ā4.
Factors significantly associated with subscapularis tendon tear in multivariable analysis
REFERENCES
1. Keating JF, Waterworth P, Shaw-Dunn J, Crossan J. The relative strengths of the rotator cuff muscles: a cadaver study. J Bone Joint Surg Br 1993;75:137ŌĆō40.


2. Kuechle DK, Newman SR, Itoi E, Morrey BF, An KN. Shoulder muscle moment arms during horizontal flexion and elevation. J Shoulder Elbow Surg 1997;6:429ŌĆō39.


4. Li XX, Schweitzer ME, Bifano JA, Lerman J, Manton GL, El-Noueam KI. MR evaluation of subscapularis tears. J Comput Assist Tomogr 1999;23:713ŌĆō7.


5. Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am 2007;89:1184ŌĆō93.


6. Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy 2008;24:997ŌĆō1004.


7. Bennett WF. Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy: arthroscopic appearance and incidence of ŌĆ£hiddenŌĆØ rotator interval lesions. Arthroscopy 2001;17:173ŌĆō80.

8. Lo IK, Burkhart SS. The etiology and assessment of subscapularis tendon tears: a case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy 2003;19:1142ŌĆō50.


9. Leite MJ, Pinho AR, Sa MC, Silva MR, Sousa AN, Torres JM. Coracoid morphology and humeral version as risk factors for subscapularis tears. J Shoulder Elbow Surg 2020;29:1804ŌĆō10.


10. Leite MJ, Sa MC, Lopes MJ, Matos RM, Sousa AN, Torres JM. Coracohumeral distance and coracoid overlap as predictors of subscapularis and long head of the biceps injuries. J Shoulder Elbow Surg 2019;28:1723ŌĆō7.


11. Cetinkaya M, Ataoglu MB, Ozer M, Ayanoglu T, Kanatli U. Subscapularis tendon slip number and coracoid overlap are more related parameters for subcoracoid impingement in subscapularis tears: a magnetic resonance imaging comparison study. Arthroscopy 2017;33:734ŌĆō42.


12. Cetinkaya M, Oner AY, Ataoglu MB, Ozer M, Ayanoglu T, Kanatli U. Lesser tuberosity cysts and their relationship with subscapularis tears and subcoracoid impingement. J Orthop Sci 2017;22:63ŌĆō8.


13. Zhang H, Zhang Q, Li ZL. Coracohumeral index and coracoglenoid inclination as predictors for different types of degenerative subscapularis tendon tears. Int Orthop 2019;43:1909ŌĆō16.


14. Mohtadi NG, Vellet AD, Clark ML, et al. A prospective, double-blind comparison of magnetic resonance imaging and arthroscopy in the evaluation of patients presenting with shoulder pain. J Shoulder Elbow Surg 2004;13:258ŌĆō65.


15. Razmjou H, Fournier-Gosselin S, Christakis M, Pennings A, ElMaraghy A, Holtby R. Accuracy of magnetic resonance imaging in detecting biceps pathology in patients with rotator cuff disorders: comparison with arthroscopy. J Shoulder Elbow Surg 2016;25:38ŌĆō44.


16. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327ŌĆō34.



17. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206ŌĆō52.


18. Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome: a new worldwide definition. Lancet 2005;366:1059ŌĆō62.


19. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735ŌĆō52.


20. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004;110:227ŌĆō39.


22. Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg 2009;1:96ŌĆō104.



23. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;(304):78ŌĆō83.

24. Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol 1998;33:163ŌĆō70.


25. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly: assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 1996;67:264ŌĆō8.


26. Deutsch A, Altchek DW, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg 1996;5:186ŌĆō93.


27. Belsley DA, Kuh E, Welsch RE. Regression diagnostics: identifying influential data and sources of collinearity. Hoboken, NJ: Wiley; 2005.
29. Wang H, Cheng Y, Shao D, et al. Metabolic syndrome increases the risk for knee osteoarthritis: a meta-analysis. Evid Based Complement Alternat Med 2016;2016:7242478.



30. Abate M, Di Carlo L, Salini V, Schiavone C. Metabolic syndrome associated to non-inflammatory Achilles enthesopathy. Clin Rheumatol 2014;33:1517ŌĆō22.


31. Park HB, Gwark JY, Im JH, Jung J, Na JB, Yoon CH. Factors associated with atraumatic posterosuperior rotator cuff tears. J Bone Joint Surg Am 2018;100:1397ŌĆō405.


32. Sakurai G, Ozaki J, Tomita Y, Kondo T, Tamai S. Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: cadaveric and clinical studies. J Shoulder Elbow Surg 1998;7:510ŌĆō5.


33. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle: clinical features in 16 cases. J Bone Joint Surg Br 1991;73:389ŌĆō94.


34. Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am 1996;78:1015ŌĆō23.

35. Kim TK, Rauh PB, McFarland EG. Partial tears of the subscapularis tendon found during arthroscopic procedures on the shoulder: a statistical analysis of sixty cases. Am J Sports Med 2003;31:744ŌĆō50.


36. Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116ŌĆō20.


37. Mehta SK, Teefey SA, Middleton W, Steger-May K, Sefko JA, Keener JD. Prevalence and risk factors for development of subscapularis and biceps pathology in shoulders with degenerative rotator cuff disease: a prospective cohort evaluation. J Shoulder Elbow Surg 2020;29:451ŌĆō8.



38. Bodin J, Ha C, Chastang JF, et al. Comparison of risk factors for shoulder pain and rotator cuff syndrome in the working population. Am J Ind Med 2012;55:605ŌĆō15.


39. Kim YK, Jung KH, Kim JW, Kim US, Hwang DH. Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: a retrospective cohort study. J Shoulder Elbow Surg 2018;27:1012ŌĆō20.


40. Cho NS, Moon SC, Jeon JW, Rhee YG. The influence of diabetes mellitus on clinical and structural outcomes after arthroscopic rotator cuff repair. Am J Sports Med 2015;43:991ŌĆō7.


41. Gaida JE, Alfredson L, Kiss ZS, Wilson AM, Alfredson H, Cook JL. Dyslipidemia in Achilles tendinopathy is characteristic of insulin resistance. Med Sci Sports Exerc 2009;41:1194ŌĆō7.


42. Longo UG, Franceschi F, Ruzzini L, Spiezia F, Maffulli N, Denaro V. Higher fasting plasma glucose levels within the normoglycaemic range and rotator cuff tears. Br J Sports Med 2009;43:284ŌĆō7.


43. Esposito K, Nappo F, Marfella R, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation 2002;106:2067ŌĆō72.


44. Reddy GK. Glucose-mediated in vitro glycation modulates biomechanical integrity of the soft tissues but not hard tissues. J Orthop Res 2003;21:738ŌĆō43.


45. Reddy GK, Stehno-Bittel L, Enwemeka CS. Glycation-induced matrix stability in the rabbit achilles tendon. Arch Biochem Biophys 2002;399:174ŌĆō80.


46. Bergin D, Parker L, Zoga A, Morrison W. Abnormalities on MRI of the subscapularis tendon in the presence of a full-thickness supraspinatus tendon tear. AJR Am J Roentgenol 2006;186:454ŌĆō9.


47. Erickson SJ, Fitzgerald SW, Quinn SF, Carrera GF, Black KP, Lawson TL. Long bicipital tendon of the shoulder: normal anatomy and pathologic findings on MR imaging. AJR Am J Roentgenol 1992;158:1091ŌĆō6.


48. Chen CH, Hsu KY, Chen WJ, Shih CH. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma 2005;58:1189ŌĆō93.


49. Adams CR, Brady PC, Koo SS, et al. A systematic approach for diagnosing subscapularis tendon tears with preoperative magnetic resonance imaging scans. Arthroscopy 2012;28:1592ŌĆō600.


50. Chae SH, Jung TW, Lee SH, et al. Hidden long head of the biceps tendon instability and concealed intratendinous subscapularis tears. Orthop J Sports Med 2020;8:2325967119898123.



- TOOLS