|
 |
- Search
| Clin Shoulder Elb > Volume 26(2); 2023 > Article |
|
Abstract
Avascular necrosis (AVN) of the humeral head is a rare, yet detrimental complication. Left untreated, humeral head AVN frequently progresses to subchondral fracturing and articular collapse. Cases of late-stage humeral head AVN commonly require invasive procedures including humeral head resurfacing, hemiarthroplasty, and total shoulder arthroplasty (TSA) to improve clinical outcomes. However, in cases of early-stage AVN, core decompression of the humeral head is a viable and efficacious short-term treatment option for patients with pre-collapse AVN of the humeral head to improve clinical outcomes and prevent disease progression. Several techniques have been described, however, a percutaneous, arthroscopic-assisted technique may allow for accurate staging and concomitant treatment of intraarticular pathology during surgery, although further long-term clinical studies are necessary to assess its overall outcomes compared with standard techniques. Biologic adjunctive treatments, including synthetic bone grafting, autologous mesenchymal stem cell/bone marrow grafts, and bone allografts are viable options for reducing the progression of AVN to further collapse in the short term, although long-term follow-up with sufficient study power is lacking in current clinical studies. Further long-term outcome studies are required to determine the longevity of core decompression as a conservative measure for early-stage AVN of the humeral head.
Avascular necrosis (AVN) of the humeral head is a rare complication. Atraumatic AVN of the humeral head is infrequently isolated, coinciding with multifocal osteonecrosis including the hip [1,2]. Following AVN, inflammation, fibrosis, and sclerosis of the humeral head occurs as the body attempts to heal the damaged bone. However, if left untreated, AVN frequently progresses to subchondral fracturing and articular collapse [3,4]. AVN symptoms of the humeral head are commonly unrecognized and non-specific in early stages prior to collapse of the humeral head, often leading to misdiagnosis and inaccurate treatment. Particularly, in a prior study, up to 71% of patients in one cohort had progression of their humeral head AVN in the setting of nonoperative management, highlighting a devastating natural history of the condition [5]. In patients with late-stage AVN, including Cruess stage III–V AVN [6], treatment often requires extensive intervention, including humeral head resurfacing [7,8], hemiarthroplasty [9,10], and total shoulder arthroplasty (TSA) [5,10], because management of the osteonecrosis is unamendable to more conservative measures. In patients with early-stage AVN, including Cruess stages I and II, several measures have been described, most notably core decompression [11-14]. Although core decompression has been well described as a viable option for management of early-stage AVN in the femoral head [15-21], outcome studies related to the humeral head have been relatively limited without complete consensus on superior techniques to optimize patient outcomes and reduce overall AVN progression.
In this article, the etiology, clinical presentation, and classification of AVN of the humeral head, the indications and current techniques for core decompression of the humeral head, and a complete summary of all current clinical outcomes for each core decompression technique, including the use of adjunctive biologics for the humeral head, are presented.
Traumatic injury of the proximal humerus is the leading cause of AVN of the humeral head. Proximal humerus fractures increase the risk of disrupting both anterior circumflex and posterior circumflex arteries, the primary vascular supply of the proximal humerus. Significant proximal humerus fracture patterns of humeral head AVN have been reported, including 0%–25% risk for three-part fractures [22-24] and 0%–77% risk for four-part fractures [22-25]. The risk of traumatic AVN has a strong correlation with initial medial hinge integrity and length of the metaphyseal head extension [26], and likely associated with displacement-induced stripping of the periosteum and vessels [27]. However, despite the fracture pattern severity, younger age has been associated with greater resistance to AVN [28].
Although consensus is lacking on the pathogenesis of atraumatic AVN of the humeral head, several theories have been presented. As previously described, AVN develops due to vascular compromise, commonly due to traumatic etiology. However, certain risk factors and genetic predisposition may increase the risk of vascular disruption, increasing the risk for osteonecrosis through increased intraosseous pressure and compromised blood supply [6,29-32]. Although cases can be idiopathic, several risk factors, both direct and indirect, have been proposed, most notably corticosteroid use [33], sickle cell anemia [31,34,35], systemic lupus erythematosus [36], alcohol consumption [37,38], human immunodeficiency virus (HIV) [39-41], and dysbaric osteonecrosis [42,43].
AVN of the humeral head is characterized by insidious onset of shoulder pain, often without evidence of an inciting event. Patients can experience significant glenohumeral pain, either at rest or with shoulder motion. Some patients may experience pain at night, limiting sleep. In addition to pain, patients may experience shoulder stiffness or weakness of the rotator cuff. In cases of advanced AVN, there may be clicking/clunking of the shoulder with movement due to either an arthritic or collapsed humeral head. Progressive AVN can lead to intraarticular osteochondral fragments, causing locking or popping. Tenderness with shoulder motion is often delayed to later stages of the disease, with most discomfort occurring with maximum glenohumeral loading at >90° of arm abduction [23].
Initial assessment in suspected AVN of the humeral head should include an extensive clinical and radiographic examination to assess for osteosclerosis, subchondral lucency, and frank joint collapse of the humeral head. A history and physical examination for suspected AVN of the humeral head should first be assessed with plain radiography. On plain films, early osteonecrosis of the humeral head is often not detected (Fig. 1). However, signs of sclerosis or cystic changes may be suggestive of underlying AVN (Fig. 2) [44]. With progression of AVN, the articular surface of the humeral head may collapse due to subchondral fracturing in the area of bone necrosis and identified on plain radiographs by the “crescent sign,” an area of subchondral lucency and incongruency of the articular surface. Later stages of AVN progress to flattening, collapse, and progressive degenerative changes [6].
After plain radiography, magnetic resonance imaging (MRI) is considered the modality of choice for the diagnosis of early-stage AVN. The benefits of MRI are associated with sensitive identification of early changes of water and fat content of the bone marrow not evident on plain radiographs [23]. Thus, in cases of suspected osteonecrosis with negative results on plain radiography, MRI of the shoulder should be performed. However, in late stages of AVN, plain radiography and occasionally computed topography (CT) imaging are recommended for further evaluation of subchondral fracturing [23].
AVN of the humeral head is most commonly classified according to the Cruess staging for osteonecrosis of the humeral head [6] as modified from the Ficat and Arlet classification of the hip [45]. In brief, the Cruess classification describes the severity of osteonecrosis of the humeral head as follows: stage I, negative findings on plain radiographs and bone marrow signal changes on MRI; stage II, plain radiographs showing focal subchondral osteolysis and/or mottled or wedged sclerosis of the superior humeral head without articular collapse; stage III, subchondral collapse and loss of humeral head sphericity, commonly associated with the “crescent sign”; stage IV, extensive subchondral bone collapse and loss of humeral head sphericity and secondary arthritic changes; stage V, progressive osteonecrosis with arthritic changes extending onto the glenoid articular surface (Fig. 3) [11]. In general, the criteria for early (stage I or II) versus late (stage III–V) stage AVN of the humeral head depends on the radiographic and clinical presence of humeral head subchondral collapse in late-stage AVN [11].
In the setting of early-stage osteonecrosis of the humeral head, including stages I and II osteonecrosis where subchondral collapse of the humeral head has not yet occurred, nonoperative management can be explored to address shoulder pain and mechanical symptoms. Prior to considering core decompression or other operative measures, management can include shoulder physical therapy for strengthening and improving range of motion, activity modification, and medical management of any underlying medical conditions that may have contributed to the development of the osteonecrosis as aforementioned. Anti-inflammatory medications may be useful for pain control. However, as previously mentioned, a high rate of progression of humeral head osteonecrosis has been emphasized in prior studies, with more than 71% of patients in mid to late stages having disease progression as early as the 2-year follow-up [5]. This reaffirms the necessity for early diagnosis and intervention to prevent further progression to later-stage AVN, including progression to subchondral collapse and further development of AVN-associated glenohumeral arthritis.
Since the introduction of core decompression by Mont et al. [13] for the treatment of the humeral head osteonecrosis, the method has been considered a viable conservative option to prevent further progression of AVN and prolong the time before extensive treatment measures, including humeral head resurfacing, hemiarthroplasty, and TSA, are performed. Although initially described for all stages of humeral head AVN, poor clinical outcomes for patients with late-stage AVN of the humeral head, primarily in Cruess stages IV and V, have been shown in clinical studies. In particular, excellent outcomes in ≥ 88% of patients with Cruess stage I or II AVN of the humeral head were reported in early studies, however, in studies by LaPorte et al. [12] and Mont et al. [36], excellent outcomes in stage III osteonecrosis were observed in only 70% of patients. Additional decline in success rates was observed in stage IV AVN, with excellent outcomes as low as 14% [12]. Furthermore, studies by L'Insalata et al. [5] described five shoulders with stage III AVN that progressed to TSA (80%) or stage IV AVN (20%). Thus, based on early evidence, whether core decompression in stage III AVN produces long-term clinical benefit is unclear because subchondral collapse has already occurred. Nevertheless, core decompression is indicated in symptomatic patients with Cruess stage I or II AVN, however, alternatives to core decompression may be considered in stages III–V depending on patient age, functional status, and consideration of arthroplasty longevity. To date, there have not been sufficient clinical studies to further clarify outcomes of core decompression of the humeral head based on other patient characteristics or preoperative shoulder patient reported outcome scores, limiting selection based on clinically symptomatic patients with radiographic signs of early-stage AVN. However, in general, core decompression should be performed in patients with early-stage AVN of the humeral head without articular collapse (Cruess stages I and II), and in patients in whom nonoperative measures including analgesics, physical therapy, and corticosteroid injections failed [44]. Several techniques have been developed for core decompression of the humeral head, and are described in detail in the following section.
A summary of available core decompression techniques and clinical outcome studies for the humeral head is presented in Table 1.
Each technique for core decompression is performed under general anesthesia with the patient either in the supine or beach chair position on a standard operating table.
Mont et al. [13] were the first to present core decompression for AVN of the humeral head using a standard technique with a 5-mm coring device (single large trephine).The standard open technique involves utilizing the deltopectoral interval. To perform the open technique, a 2-cm incision is made superior to the pectoralis major tendon anterior to the axillary fold. The deltopectoral interval is developed by blunt dissection until the proximal humerus is reached. Care should be taken to not disrupt the common neurovascular structures within the interval [50]. A single coring device is then utilized and drilled into the proximal humeral metaphysis slightly lateral to the bicipital groove. Accurate decompression should be confirmed with intraoperative fluoroscopy corresponding to the lesion position observed on preoperative imaging. Although originally described with a 5 mm trephine, several other techniques have been developed with single trephines ranging from 6 mm–10 mm in size [12,13,36].
Mont et al. [13] reported good to excellent University of California Los Angeles (UCLA) shoulder score outcomes for core decompression of Ficat and Arlet [45] stage I or stage II humeral head AVN with no progression to TSA. Conversely, 3 of 10 stage III and 5 of 6 stage IV shoulders progressed to TSA, with the 1 stage IV shoulder not progressing to TSA having an outcome of only good. Similar results were observed in follow-up studies by LaPorte et al. [12] and Mont et al. [36], with excellent outcomes of early-stage humeral head AVN and high failure rates in shoulders with stage III–V AVN. This was consistent with studies by L'Insalata et al. [5] in which all five shoulders with stage III AVN progressed to TSA (80%) or stage IV AVN (20%).
Although the traditional technique for core decompression has been shown an effective technique for both the hip and humeral head, a small-diameter percutaneous technique showed excellent results for core decompression of the hip [16,51]. The inception of this technique was based on the theory that multiple passes into the necrotic lesion will increase the coverage of the necrotic lesion, and the percutaneous technique reduces surgical morbidity in comparison with the larger surgical incisions required for a large trephine. More recently, the technique has been adapted for the humeral head [11]. In brief, the technique by Harreld et al. [11] utilizes multiple small diameter percutaneous perforations using a 3.2-mm Steinmann pin advanced twice, for smaller lesions, or three times for larger lesions, to the epiphyseal lesion under fluoroscopic guidance (Fig. 4). Insertion of the Steinmann pin should be localized lateral to the bicipital groove, reducing risk of damage to the ascending branch of the anterior humeral circumflex artery [52]. Kennon et al. [10] also presented this technique utilizing a standard 2.7-mm drill bit passed several times into the necrotic lesion under fluoroscopic guidance. Although a small-diameter drill is more commonly used, a single large trephine may also be utilized for the percutaneous technique albeit with a larger initial incision to accommodate the larger drill (Fig. 5). The authors recommend a lateral approach when a larger drill, reamer, or trephine is used. Under fluoroscopy, a lateral point of entry inferior to the level of the axillary nerve is localized using a spinal needle. An incision is then made and a blunt dissection performed down to the lateral cortex of the proximal humerus. A blunt trocar can then be used for dilation of the incision and to reduce risk of iatrogenic nerve injury. Next, a standard core decompression with a large trephine is performed as previously described.
Harreld et al. [11] assessed the outcomes of patients with Cruess stage I or stage II AVN of the humeral head treated with percutaneous core decompression. In a cohort of 15 patients (26 shoulders), the mean UCLA shoulder scores increased from 14 (range, 10–22) preoperatively to 27 (range, 14–30) postoperatively at the mean follow-up of 32 months (range, 24–41 months). Only 1 patient had poor outcome with a UCLA score of 11 preoperatively and 14 postoperatively, however, this patient was complicated by spondyloarthropathy and multiple joint involvement of the AVN.
Although good outcomes for core decompression were observed in previous studies, mixed results were reported in a case series by Kennon et al. [10] in which 11 patients (11 shoulders) with stage I or stage II humeral head AVN were assessed for outcomes following core decompression. The procedure was performed using a standard 2.7-mm drill bit with multiple fluoroscopically guided passes with concurrent intraoperative ultrasound bone stimulation. Among the 11 patients, 3 were lost to 1-year follow-up. However, two of three patients continued to have persistent pain postoperatively. At the mean follow-up of 17.4 months, seven of the eight remaining patients progressed to further collapse and five required additional resurfacing procedures due to continued postoperative symptoms. Functional outcomes in that study were only assessed following resurfacing, TSA, or reverse TSA, however, the high failure rate and progression within 2 years postoperatively raises concerns for long-term durability of the procedure.
The use of arthroscopy in core decompression of the humeral head was first introduced by Chapman et al. [53] as an adjunctive measure for accurate articular assessment and placement of the guide pin. The main premise of this technique is to reduce the risk of iatrogenic perforation of the articular surface while additionally allowing the surgeon to treat coinciding shoulder pathology, including synovitis and chondral pathology, which may limit optimal postoperative recovery. Furthermore, arthroscopy provides the benefit of direct observation of articular surface collapse without the need of an open incision. In brief, arthroscopic-assisted core decompression is performed using two standard portals, including posterior and anterior portals. After the arthroscope is placed in the posterior portal, a standard diagnostic arthroscopy is performed with full assessment of the intraarticular cartilage, labrum, rotator cuff, biceps, and subacromial bursa. During the arthroscopy, any intraarticular pathology should be appropriately managed. In addition, arthroscopy allows for the absence of humeral head collapse, which would contraindicate core decompression, to be confirmed. Once diagnostic arthroscopy is complete, a lateral portal is established and a standard percutaneous core decompression is completed. Intraoperatively, the arthroscope is maintained within the posterior portal to confirm the drill has not disrupted the articular surface of the humeral head.
In addition, the use of an anterior cruciate ligament (ACL) tibial drill guide has been described an effective tool for accurate triangulation of the humeral head AVN lesion while reducing the risk of unnecessary drilling [46,49]. Dines et al. [46] described the technique in terms of a standard arthroscopic-assisted core decompression with use of only the anterior and posterior arthroscopic portals, however, the authors prefer a laterally directed mini-open incision for placement of the ACL targeting guide (Fig. 6). Due to the proximity of the axillary nerve in this anatomic area, the incision should be carefully extended down to the lateral cortex of the humerus. Fluoroscopic imaging is used to localize the necrotic lesion and the ACL tibial drill guide is positioned to triangulate the area of necrosis. Next, a soft tissue protector is placed within the incision and a guide pin is drilled into the lesion. Direct visualization using arthroscopy and fluoroscopy is performed to confirm the lesion has been reached and the pin has not penetrated through the subchondral bone into the cartilage. Then, using a 4-mm cannulated drill, a decompression channel is created by aligning with the ACL guide (Fig. 6). The guide is then moved two to three more times with concurrent drilling as described to achieve appropriate spread within the lesion. Then, the humeral head cartilage should be reinspected to ensure iatrogenic penetration has not occurred.
Dines et al. [46] reported the outcomes of 3 patients (3 shoulders) that underwent arthroscopic-assisted core decompression as first described by Chapman et al. [53]. Their technique included the use of an ACL tibial drill guide to reduce the risk of articular perforation. All three patients presented with Cruess stage II humeral head AVN based on preoperative radiographs and MRI. At an average follow-up of 9 months (range, 7–11 months), two of three patients had complete resolution of their preoperative pain, and shoulder range of motion was completely restored in three of three patients. One patient presented with persistent pain at the 9-month follow-up, although this was completely resolved with a corticosteroid injection. Long-term outcomes for this technique with and without the use of an ACL tibial drill guide are not currently available for the humeral head.
More recently, significant focus has been on the concurrent use of growth and differentiation-inducing agents following core decompression to promote native bone regeneration of the decompressed tract. In particular, methods including autologous bone grafting [15], tantalum rod implants [54-56], autologous bone marrow cell implants [57], and synthetic calcium sulfate/calcium phosphate bone cementing [58-64] have been described for core decompression in the femoral head. Although current literature on biologics for core decompression of the humeral head is limited, several techniques have been proposed.
As presented by Steffensmeier et al. [47], the use of a calcium sulfate and calcium phosphate synthetic bone graft (Pro-Dense, Wright Medical Group, Memphis, TN, USA) is a viable option for adjunctive management with core decompression. Although not sufficiently studied for the humeral head, synthetic bone graft has been proven to promote bone regeneration following femoral head AVN [65,66]. The technique is performed following a standard percutaneous core decompression. Through the original percutaneous incision, an extension cannula is placed at the decompression tract and synthetic bone graft is injected into the proximal humerus (Fig. 7). Fluoroscopy is utilized to visualize complete cementation of the decompression tract. Arthroscopy with irrigation is recommended to ensure no cement is present within the subacromial space.
Steffensmeier et al. [47] reported on one patient (two shoulders) with early-stage AVN of the humeral head who underwent core decompression with synthetic bone graft cement (Pro-Dense, Wright Medical Group). Improvement in pain and range of motion was observed at the final follow-up of 8 months for 1 shoulder and mild residual stiffness was observed at the 4-month follow-up. Neither shoulder progressed to collapse and pain in both shoulders was resolved.
The use of autologous mesenchymal cell grafts for core decompression of the femoral head has been well described. In a meta-analysis by Li et al. [57], improved outcomes were observed in patients receiving congruent mesenchymal injections compared with core decompression alone. Makihara et al. [48] recently showed this technique was a viable adjunctive treatment for core decompression of the humeral head. Bone marrow aspiration, centrifugation, and transplantation were performed according to the technique by Yoshioka et al. [67] for the femoral head. In brief, under general anesthesia, bone marrow aspirate is harvested using a bone marrow biopsy needle with an acid citrate dextrose containing syringe. Centrifugation is performed twice. The first centrifugation is performed at 1,200 ×g for 10 minutes to remove the red blood cell layer. Following a second centrifugation at 3,870 ×g for 7 minutes, the blood plasma is removed, leaving buffy coats containing the mesenchymal cell grafts. After standard percutaneous core decompression, the autologous concentrated bone marrow graft is grafted with a cylindrical rod smaller in diameter than the diameter of the drill to ease implantation. The graft is then implanted within the decompression tract. The procedure is completed by closing the incision using standard technique.
Makihara et al. [48] reported four patients (five shoulders) who underwent core decompression for four shoulders with Cruess stage III and 1 shoulder with stage IV AVN of the humeral head using autologous concentrated bone marrow grafts. At an average final follow-up of 49.4 months (range, 24–73 months), the average visual analog scale changed from 33 mm preoperatively to 5 mm postoperatively, and progression to further collapse or TSA did not occur. However, the patient with stage IV shoulder failed to improve following core decompression, requiring TSA prior to the final follow-up. Similarly, Hernigou et al. [68] reported the outcomes of 30 patients (30 shoulders) with adjunctive mesenchymal stem cell injection and 34 patients (34 shoulders) with no adjunctive injection who underwent core decompression for AVN of the humeral head. In the mesenchymal group, 18 patients were pre-collapse and 12 patients were post-collapse. At an average of 7-year follow-up (range, 5–10 years), 3 of 30 patients in the mesenchymal group progressed to humeral head collapse compared with 25 of 34 patients in the untreated group (P<0.0001). In addition, only 2 of 30 patients in the mesenchymal group progressed to shoulder arthroplasty compared with 25 of 34 in the untreated group (P<0.0001).
Galloway et al. [49] described bone allograft in conjunction with core decompression of the humeral head with use of a fibular allograft strut. Bone allograft is used to support the subchondral bone and decrease the risk of articular collapse following AVN lesion decompression rather than bony revascularization [49]. Following a standard arthroscopic-assisted percutaneous core decompression, a bone allograft is prepared with the same diameter of the drilled decompression tract. Introduction of the bone allograft is conducted over the previously placed guide pin and the pin is removed once the graft is secured. The remaining graft is then cut flush with the outer cortex with all edges smoothed using a burr. Galloway et al. [51] recommend under-contouring the graft progressing from proximal to distal to aid with interference fit of the graft within the tract.
In a study including 14 pre-collapse shoulders (stage II) and 6 post-collapse shoulders (2 stage III and 4 stage IV), Galloway et al. [49] reported good outcomes for core decompression with adjunctive fibular strut allograft. Prior to the final follow-up, 3 shoulders, including 2 stage II and 1 stage IV, underwent shoulder arthroplasty due to pain. In the pre-collapse group, Shoulder Disability and Shoulder Pain and Disability Index (SPADI) scores were excellent in two shoulders, good in four shoulders, and poor in one shoulder. In contrast, SPADI scores in the post-collapse group included three excellent and one poor result. Limited improvement was observed in range of motion for both groups postoperatively. The better outcome scores in the post-collapse group were attributed to the younger patient age compared with pre-collapse group.
In the literature searched, formal consensus on postoperative restrictions following core decompression was not found. In a few articles, a short period of several days of sling immobilization with early progressive range of motion and limited heavy lifting for 8–12 weeks was recommended [11-13]. Conversely, Steffensmeier et al. [47] recommended no formal postoperative restrictions aside from tolerated activity and Makihara et al. [48] only recommended limiting carrying loads following core decompression. Although postoperative protocols differ, formal evidence indicating the gold standard for postoperative rehabilitation does not exist. However, the concern for postoperative stiffness and functional limitations should be considered with any postoperative protocol. Thus, the authors recommend patients begin a postoperative protocol with early range of motion, including shoulder pendulums, elbow, wrist, and hand exercises, to reduce stiffness. However, restrictions should be guided based on concomitant procedures. If the operation is an isolated core decompression, the authors recommend no formal restrictions and patients allowed to return to their normal activity level as tolerated.
Core decompression of the humeral head is an excellent treatment modality for shoulder preservation in patients with early-stage AVN of the humeral head without articular collapse. Several techniques have been developed, with good to excellent outcomes for each modality. In theory, a percutaneous, arthroscopic-assisted technique may allow accurate staging and concomitant treatment of intraarticular pathology during surgery, although further long-term clinical studies are necessary to assess the overall outcomes compared with standard techniques. In addition, although use of adjunctive biologics has been well described for core decompression of the hip, further high-quality studies are required in which their benefit in core decompression of the humeral head is further assessed.
NOTES
Author contributions
Conceptualization: MDS, SA, DS, NG. Visualization: MDS. Writing – original draft: MDS, SA, DS, NG. Writing – review & editing: MDS, SA, DS, NG.
Fig. 1.
Illustration depicting the Cruess staging of osteonecrosis of the humeral head. Stage I, no evident changes on radiographic imaging with bone marrow changes only observed on magnetic resonance imaging; stage II, plain radiographs showing focal subchondral osteolysis and/or mottled or wedged sclerosis of the superior humeral head without articular collapse; stage III, subchondral collapse and loss of humeral head sphericity, commonly associated with the “crescent sign”; stage IV, extensive subchondral bone collapse and loss of humeral head sphericity and secondary arthritic changes; stage V, progressive osteonecrosis with arthritic changes extending onto the glenoid articular surface.
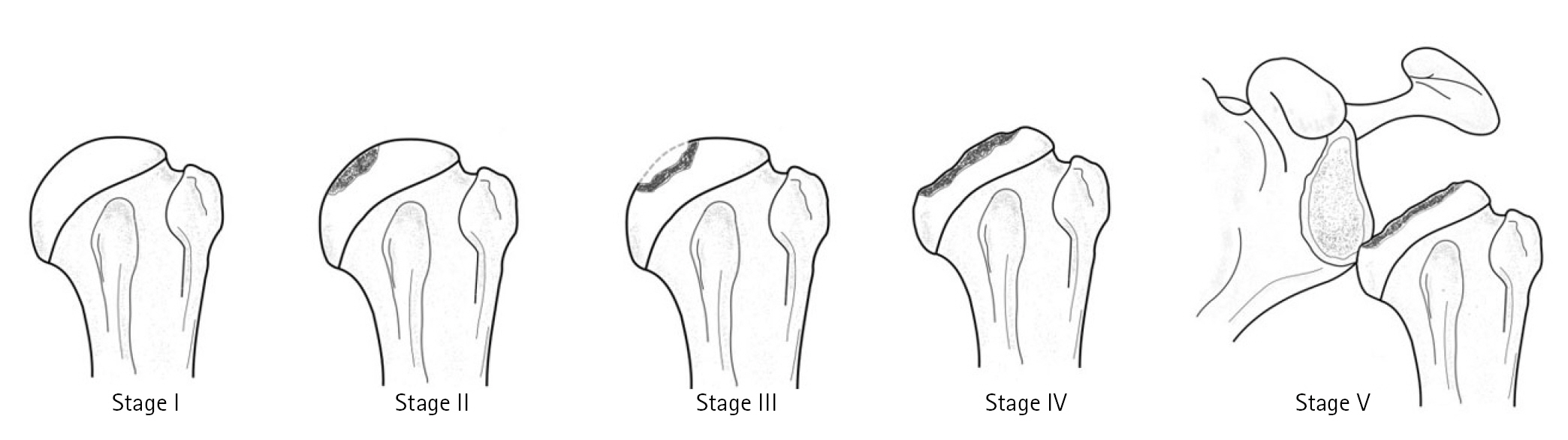
Fig. 2.
Preoperative plain anterior-posterior with internal rotation and T2-weighted coronal magnetic resonance imaging (MRI) of the shoulder showing stage I avascular necrosis of the humeral head. (A) The plain radiographic view of the shoulder showing absent osteosclerosis or articular abnormality. (B) T2-weighted MRI showing a T2 signal intensity of the medial humeral head, consistent with osteonecrosis.
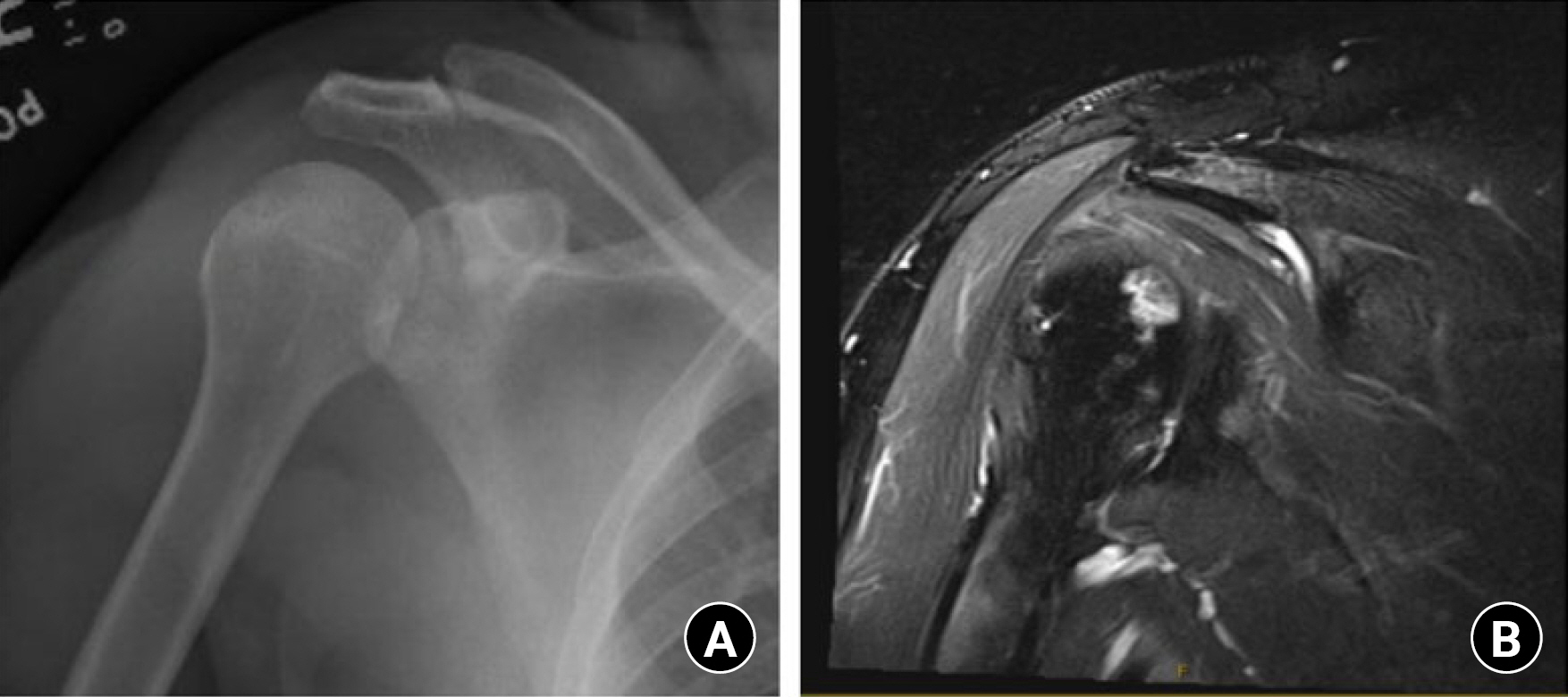
Fig. 3.
Preoperative plain anterior-posterior radiograph (A) and sagittal T2 magnetic resonance imaging (MRI; B) view of the shoulder showing stage II avascular necrosis (AVN) of the humeral head. Plain radiographic views of the right shoulder and right humerus show diffuse osteosclerosis consistent with AVN. (A) A subtle subchondral linear lucency at the humeral head without frank collapse is present. (B) T2-weighted MRI showing a focal region of subchondral osteonecrosis of the humeral head with areas of increased T2 signal and a subchondral fracture line without humeral head collapse.
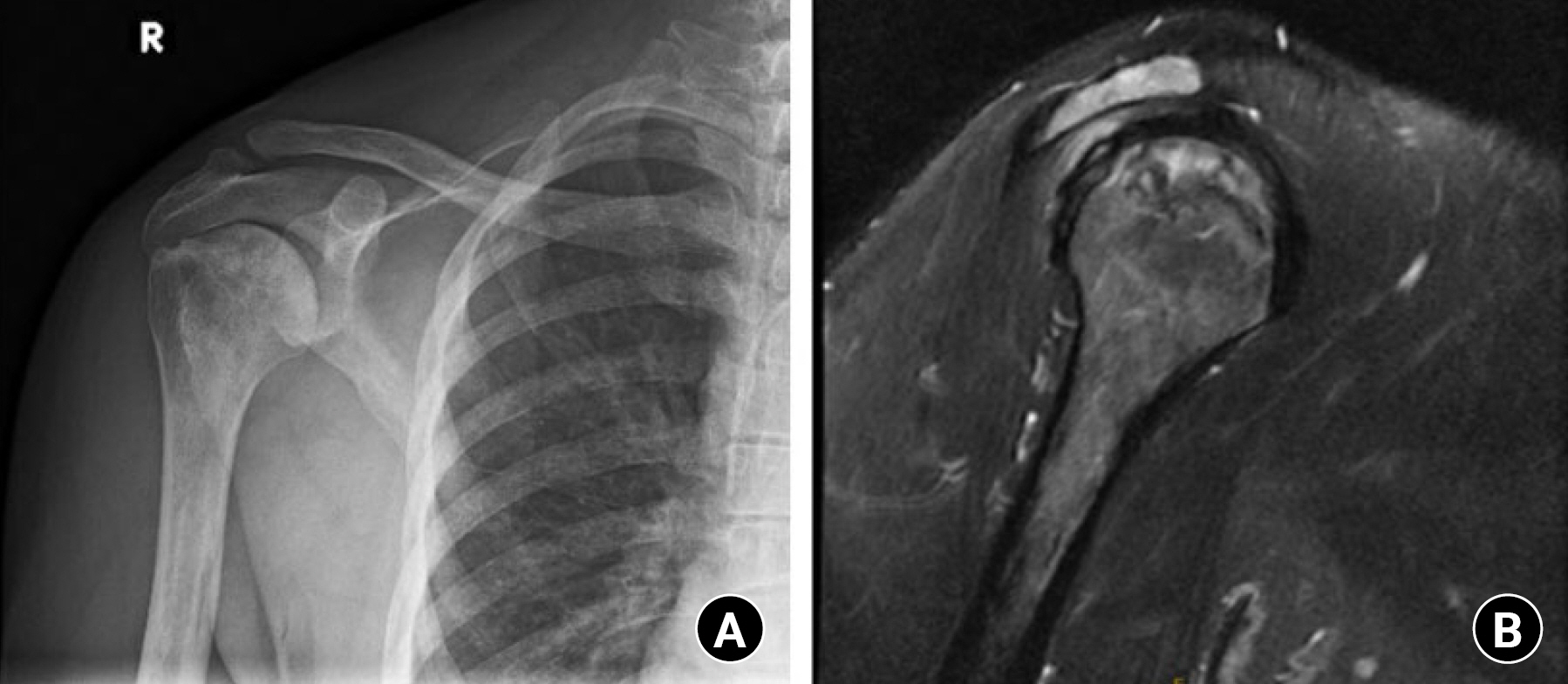
Fig. 4.
Right shoulder, beach chair position. Illustration of small-diameter percutaneous core decompression of the humeral head using a 3.5-mm drill bit. (A) Under fluoroscopic guidance, the area of necrosis is identified. (B-D) Several passes with the drill are then made into the necrotic lesion, creating 2–4 decompression tracts.
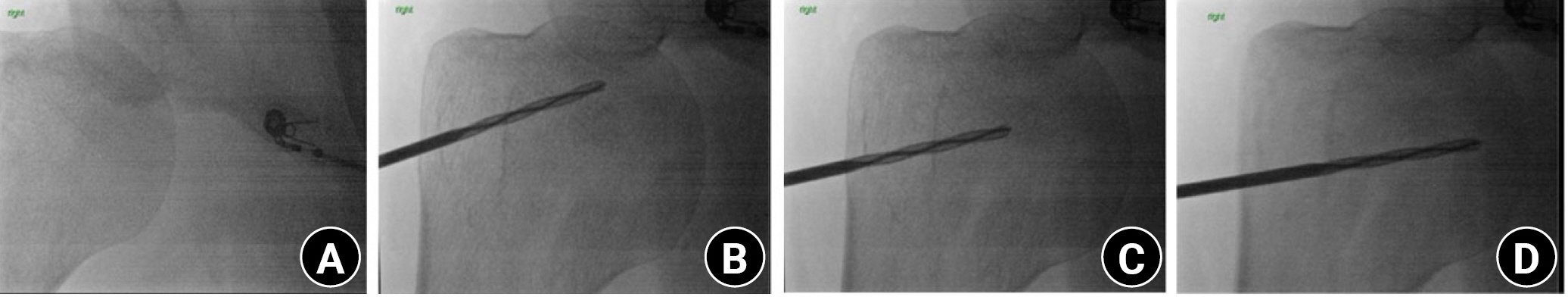
Fig. 5.
Right shoulder, beach chair position. Illustration of core decompression using a 9-mm reamer. (A) Placement of the guide pin within the humeral head. The guide pin is directionally placed from a lateral approach, directed under fluoroscopic guidance to the necrotic lesion. (B) The avascular necrosis lesion is then over-reamed using a 9-mm diameter reamer with a single pass.
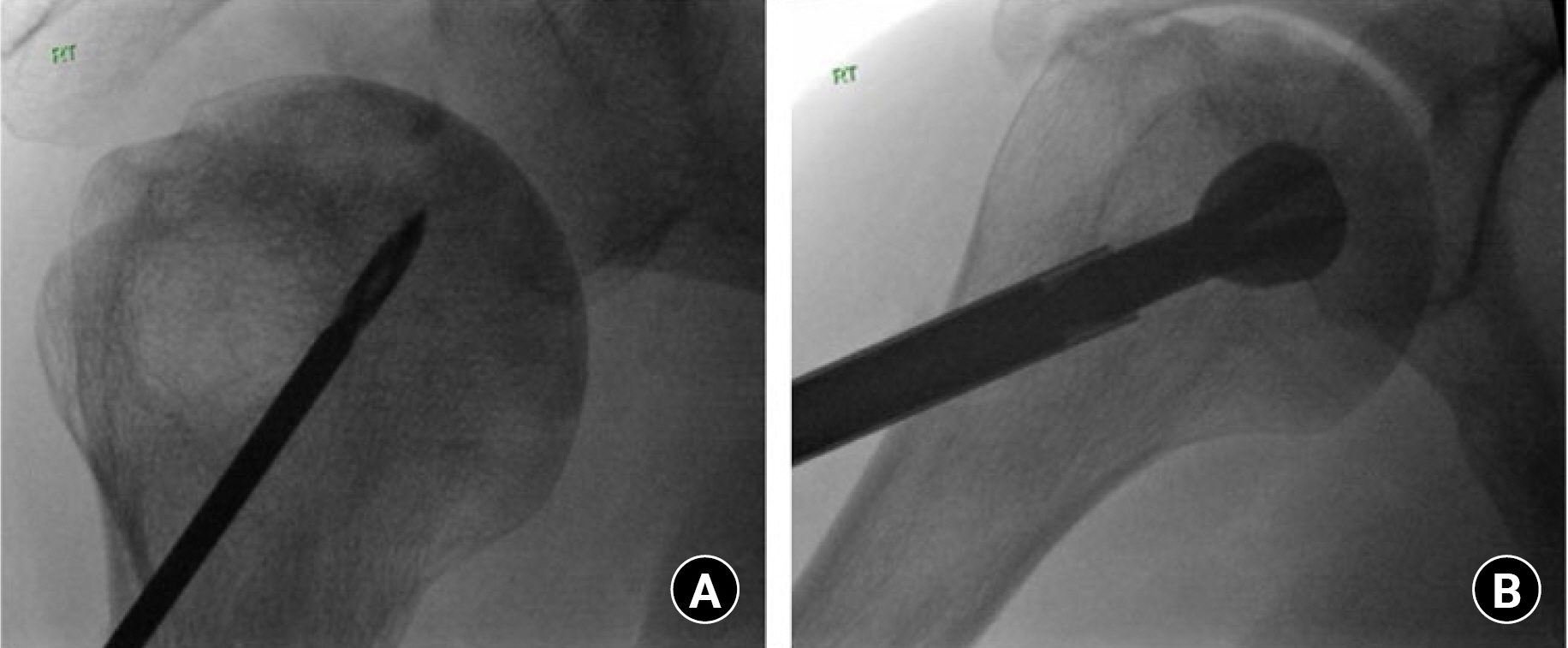
Fig. 6.
Right shoulder, beach chair position. Intraoperative fluoroscopic imaging depicting percutaneous core decompression of the humeral head using an anterior cruciate ligament (ACL) tibial guide. (A) An ACL tibial drill guide is positioned through a lateral portal to triangulate the area of necrosis on the humeral head. (B) A soft tissue protector is then placed within the incision and a guide pin is drilled into the lesion. (C) With a 4-mm cannulated drill, a decompression channel is created by aligning with the ACL guide. The guide is then moved two to three more times with concurrent drilling as described to achieve appropriate spread within the lesion.
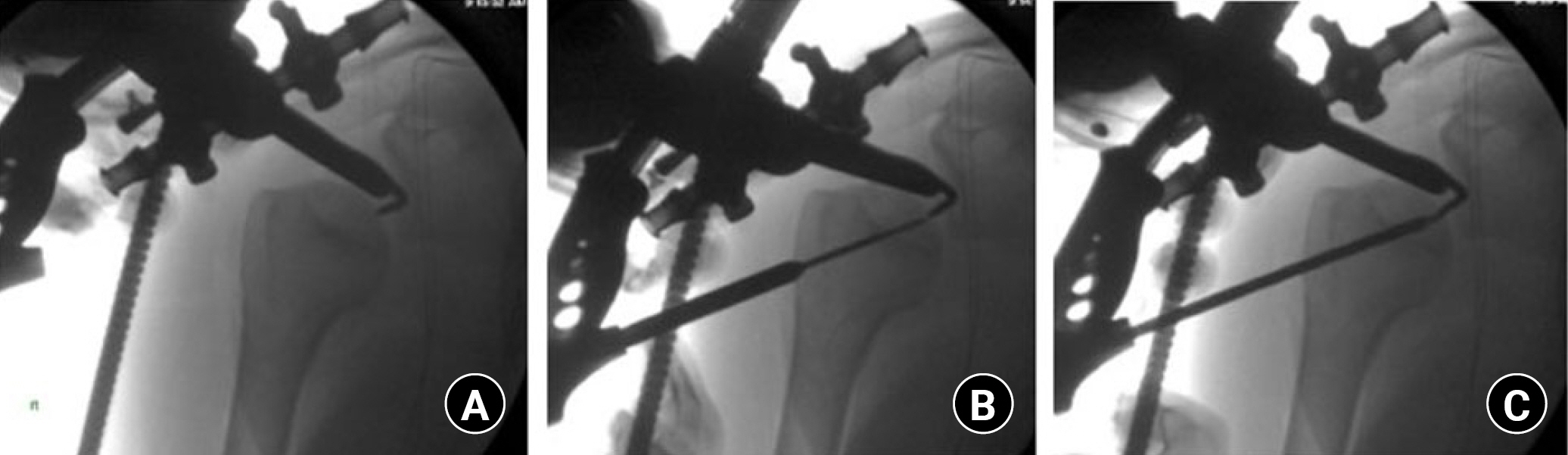
Fig. 7.
Right shoulder, beach chair position. Intraoperative fluoroscopic imaging demonstrating core decompression with synthetic bone grafting. (A) Through the original percutaneous incision, an extension cannula is place at the decompression tract and synthetic bone graft is injected into the proximal humerus. (B, C) Fluoroscopy is used to visualize complete cementation of the decompression tract. Arthroscopy with irrigation is recommended to ensure no cement is present within the subacromial space.
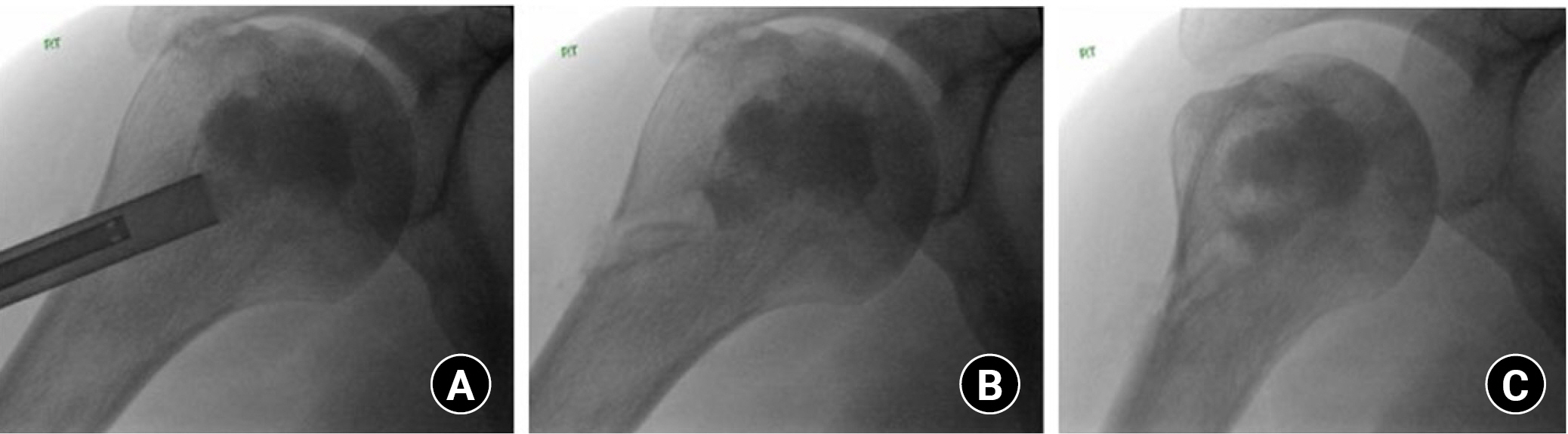
Table 1.
Clinical outcome studies for core decompression of the humeral head
| Study | Study type | No. of patients (shoulders) | Age (range, yr)/sex | Follow-up (range) | Procedure | Graft | Disease stage | Outcome | Complication/ advancement of disease |
|---|---|---|---|---|---|---|---|---|---|
| Mont et al. (1993)a) [13] | Retrospective review | 20 (30) | 38 (22–76)/5.6 yr | 11 F, 9 M | 5-mm diameter coring device (single large trephine) | No graft | Six shoulders had stage I changes, | UCLA shoulder rating systemc): 20 excellent, 2 good, 8 poor requiring hemi or TSA; all shoulders with initial stage I or II (n=14) had good or excellent; at time of follow-up, 11/14 stage I or II deteriorated radiologically; of 10 stage III—7 with excellent, 3 with arthroplasty; of stage IV, 1 with good and 5 requiring arthroplasty | 5/6 Stage IV progressed to TSA |
| 8 stage II, 10 stage III, and 6 stage IVb) | |||||||||
| L'Insalata et al. (1996) [5] | Retrospective review | 4 (5) | Not indicated | Range, 1 mo–4 yr | Humeral head drilling | No graft | Stage IIIb) | Not indicated | 4/5 Progressed to arthroplasty at intervals of 1 month, 1 year, 1 year, and 3 years; fifth shoulder with progression to stage IV |
| LaPorte et al. (1998)a),d)[12] | Retrospective review | 43 (63) | CSI group: 37 (22–60)/ 20 F 14 M; Non-CSI group: 41 (23-78)/ 4 F 5 M | 10 yr (2–20) | Single large trephine, percutaneous fluoroscopic guided core decompression | No graft | CSI groupb): stage I, 14; stage II, 13; stage III, 18; stage IV, 5 Non-CSI group: stage I, 2; stage II, 4; stage III, 5; stage IV, 2 | Average preoperative and postoperative UCLA shoulder scoresc) based on stage; stage 1, 17–27; stage 2, 15–27; stage 3, 14–25; stage 4, 12–20 | 16 Shoulders (1 stage I, 2 stage II, 7 stage III, 6 stage IV) required shoulder arthroplasty |
| Mont et al. (2000)a) [36] | Retrospective review | 95 Shoulders | Total project: 41 yr (20-60)/ 47 F 26 M; Core decompression specific not listed | 6 yr (2–21) | 5-mm diameter coring device (single large trephine) | No graft | Stage I, 16; stage II, 37; stage III, 34; stage IV, 8b) | UCLA shoulder rating systemc): stage I, 15/16 successful clinical outcomes; stage II, 34/37 successful; stage III, 24/34 successful; 9 shoulders improved to stage II; stage iV, 1/8 successful | No complications from core decompression; 8 stage II progressed to stage III; 12 stage III progressed to stage IV |
| Harreld et al. (2009) [11] | Retrospective review | 15 (26) | 37 (15–50)/7 F, 8 M | 32 mo (24-41) | Percutaneous small-diameter perforations technique under fluoroscopy guidance | No graft | Stage I/IIe) (as modified by Cruess) | UCLA shoulder rating systemc): mean score: preoperative, 14 (10–22) and postoperative, 27 (14–30) | 1 Patient with spondyloarthropathy had poor outcome (11→14 postop) although with multijoint involvement |
| Kennon et al. (2016) [10] | Case series | 11 (11) | Total in study: 37.3±15.3/15 F, 5 M | 8/11 1-yr FU; 2/3 of those lost had persistent shoulder pain | Core decompression with ultrasound bone stimulation | No graft | Stage I/IIe) | 6/6 of SCD and 1/2 of CSI progressed to further collapse (mean time of 17.4 months); functional scores only assessed following resurfacing, TSA, or RTSA | 5 Required further resurfacing procedures due to continued symptoms at mean of 12.9 months |
| Dines et al. (2007) [46] | Case report | 3 (3) | 37, 49, 36/3 F | Patient 1: 7 mo; patient 2: 9 mo; patient 3: 11 mo | Arthroscopic-assisted core decompression with ACL tibial drill guide | No graft | Stage II | Final FU: patient 1, FF 165°; Ext rot, 85°; IR T12, no pain medication for shoulder; patient 2, IR T12 final follow-up; patient 3, no pain medication at final follow-up, range of motion was same as prior to surgery | Patient 2: persistent pain at 9 month FU, resolved with injection of Decadron and xylocaine |
| Steffensmeier et al. (2016) [47] | Case report | 1 (2) | 51/F | 8 mo (shoulder 1); 4 mo (shoulder 2) | Arthroscopic-assisted core decompression | Synthetic bone grafting (Pro-Dense, Wright Medical) | Extensive subchondral osteonecrosis without joint collapse - bilateral; staging not indicated | Asymptomatic with full range of motion (shoulder 1); mild residual stiffness (shoulder 2) | None |
| Makihara et al. (2017) [48] | Case report | 4 (5) | 48 (38–63)/ 3 F, 1 M | 49.4 mo (24–73) | Percutaneous fluoroscopic guided core decompression | Autologous concentrated bone marrow | Stage III, 4; stage IV, 1e) | Stage III: average change of VAS from 33 mm preoperative to 5 mm postoperative; stage IV: failed joint sparing requiring TSA at 20 months post-index procedure | Stage IV shoulder requiring TSA at 20 months post-index procedure |
| Hernigou et al. (2020) [23] | Retrospective review | 30 (30) Mesenchymal cell treated; 34 (34) matched pair control group | 46.5 (28–60)/24 F, 37 M | 7 yr (5–10) | Percutaneous Core decompression | Mesenchymal cell injection (30/64 patients); untreated simple core-decompression (34/64) | Mesenchymal cell treatede): stage I, 8; stage II, 10; stage III, 7; stage IV, 5 | Average improvements in constant scores of 40 (35–56) to 71 (50–88) in cell therapy group and 43 (31–60) to 57 (43–70) in untreated (P=0.01); average improvement in VAS scores of 45.8±7.2 to 16±3.2 in cell therapy group and 43.2±8.5 to 29±4.1 in untreated group (P=0.01) | 3/30 Mesenchymal treated progressed to collapse vs. 25/34 in untreated group (P<0.0001); 2/30 mesenchymal treated progressed to arthroplasty vs. 25 in untreated group |
| Galloway et al. (2013) [49] | Retrospective review | 14 (17) | Precollapse: 44 (33–61); postcollapse 30 (19–40) | postcollapse: 7 yr (3–18); postcollapse: 2.4 yr (1.5–3) | Arthroscopic-assisted core decompression | Fibular strut Allograft | 8 Precollapsee) (stage I and stage II); 6 postcollapse (2 stage III and 4 stage IV) | Precollapse SPADI scoresf): 1 poor, 4 good, 2 excellent; postcollapse SPADI scores: one poor, 3 excellent, 4 missing outcome scores | 2 Stage II and 1 stage IV progressed to hemiarthroplasty |
UCLA: University of California Los Angeles, TSA: total shoulder arthroplasty, CSI: corticosteroid injection, FU: follow-up, SCD: sickle cell disease, RTSA: reverse total shoulder arthroplasty, FF: forward Flexion, Ext: external rotation, IR: internal rotation, VAS: visual analog scale, SPADI: Shoulder Disability and Shoulder Pain and Disability Index.
c) UCLA shoulder rating system. Ten points assigned for each of three categories; pain, function and active movement with max of 30; excellent 27 or more, good is 24–26, fair 21–23, poor <21;
d) 20 (30) from Mont et al. (1993) [13
REFERENCES
1. Cruess RL. Corticosteroid-induced osteonecrosis of the humer¬al head. Orthop Clin North Am 1985;16:789–96.
2. LaPorte DM, Mont MA, Mohan V, Jones LC, Hungerford DS. Multifocal osteonecrosis. J Rheumatol 1998;25:1968–74.

3. Loebenberg MI, Plate AM, Zuckerman JD. Osteonecrosis of the humeral head. Instr Course Lect 1999;48:349–57.

4. Usher BW Jr, Friedman RJ. Steroid-induced osteonecrosis of the humeral head. Orthopedics 1995;18:47–51.

5. L'Insalata JC, Pagnani MJ, Warren RF, Dines DM. Humeral head osteonecrosis: clinical course and radiographic predictors of outcome. J Shoulder Elbow Surg 1996;5:355–61.


6. Cruess RL. Experience with steroid-induced avascular necrosis of the shoulder and etiologic considerations regarding osteone¬crosis of the hip. Clin Orthop Relat Res 1978;(130):86–93.


7. Levy O, Tsvieli O, Merchant J, et al. Surface replacement arthro¬plasty for glenohumeral arthropathy in patients aged younger than fifty years: results after a minimum ten-year follow-up. J Shoulder Elbow Surg 2015;24:1049–60.


8. Raiss P, Kasten P, Baumann F, Moser M, Rickert M, Loew M. Treatment of osteonecrosis of the humeral head with cement¬less surface replacement arthroplasty. J Bone Joint Surg Am 2009;91:340–9.


9. Franceschi F, Franceschetti E, Paciotti M, et al. Surgical man¬agement of osteonecrosis of the humeral head: a systematic re¬view. Knee Surg Sports Traumatol Arthrosc 2017;25:3270–8.


10. Kennon JC, Smith JP, Crosby LA. Core decompression and ar¬throplasty outcomes for atraumatic osteonecrosis of the humer¬al head. J Shoulder Elbow Surg 2016;25:1442–8.


11. Harreld KL, Marulanda GA, Ulrich SD, Marker DR, Seyler TM, Mont MA. Small-diameter percutaneous decompression for osteonecrosis of the shoulder. Am J Orthop (Belle Mead NJ) 2009;38:348–54.


12. LaPorte DM, Mont MA, Mohan V, Pierre-Jacques H, Jones LC, Hungerford DS. Osteonecrosis of the humeral head treated by core decompression. Clin Orthop Relat Res 1998;(355):254–60.

13. Mont MA, Maar DC, Urquhart MW, Lennox D, Hungerford DS. Avascular necrosis of the humeral head treated by core de¬compression: a retrospective review. J Bone Joint Surg Br 1993;75:785–8.

14. Sahajpal DT, Zuckerman JD. Core decompression for nontrau¬matic osteonecrosis of the humeral head: a technique article. Bull NYU Hosp Jt Dis 2008;66:118–9.


15. Hua KC, Yang XG, Feng JT, et al. The efficacy and safety of core decompression for the treatment of femoral head necrosis: a systematic review and meta-analysis. J Orthop Surg Res 2019;14:306.

16. Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA. Do modern techniques improve core decompression outcomes for hip osteonecrosis. Clin Orthop Relat Res 2008;466:1093–103.



17. Mazières B, Marin F, Chiron P, et al. Influence of the volume of osteonecrosis on the outcome of core decompression of the femoral head. Ann Rheum Dis 1997;56:747–50.



18. Mont MA, Jones LC, Pacheco I, Hungerford DS. Radiographic predictors of outcome of core decompression for hips with os¬teonecrosis stage III. Clin Orthop Relat Res 1998;(354):159–68.



19. Iorio R, Healy WL, Abramowitz AJ, Pfeifer BA. Clinical out¬come and survivorship analysis of core decompression for early osteonecrosis of the femoral head. J Arthroplasty 1998;13:34–41.

20. Yoon TR, Song EK, Rowe SM, Park CH. Failure after core de¬compression in osteonecrosis of the femoral head. Int Orthop 2001;24:316–8.


21. Pierce TP, Jauregui JJ, Elmallah RK, Lavernia CJ, Mont MA, Nace J. A current review of core decompression in the treat¬ment of osteonecrosis of the femoral head. Curr Rev Musculo-skelet Med 2015;8:228–32.



22. Patel S, Colaco HB, Elvey ME, Lee MH. Post-traumatic osteone¬crosis of the proximal humerus. Injury 2015;46:1878–84.



23. Hernigou P, Hernigou J, Scarlat M. Shoulder osteonecrosis: pathogenesis, causes, clinical evaluation, imaging, and classifi¬cation. Orthop Surg 2020;12:1340–9.


24. Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treat¬ment of three and four-part proximal humeral fractures. J Bone Joint Surg Am 2009;91:1689–97.



25. Greiner S, Kääb MJ, Haas NP, Bail HJ. Humeral head necrosis rate at mid-term follow-up after open reduction and angular stable plate fixation for proximal humeral fractures. Injury 2009;40:186–91.


26. Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of hu¬meral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 2004;13:427–33.


27. Resch H, Povacz P, Fröhlich R, Wambacher M. Percutaneous fixation of three-and four-part fractures of the proximal humer¬us. J Bone Joint Surg Br 1997;79:295–300.


28. Crosby LA, Finnan RP, Anderson CG, Gozdanovic J, Miller MW. Tetracycline labeling as a measure of humeral head viabil¬ity after 3- or 4-part proximal humerus fracture. J Shoulder El-bow Surg 2009;18:851–8.


29. Hattrup SJ, Cofield RH. Osteonecrosis of the humeral head: re¬lationship of disease stage, extent, and cause to natural history. J Shoulder Elbow Surg 1999;8:559–64.

30. Jones JP Jr. Concepts of etiology and early pathogenesis of os¬teonecrosis. Instr Course Lect 1994;43:499–512.


31. Chung SM, Ralston EL. Necrosis of the humeral head associated with sickle cell anemia and its genetic variants. Clin Orthop Relat Res 1971;80:105–17.

32. Jacobs B. Epidemiology of traumatic and nontraumatic osteonecrosis. Clin Orthop Relat Res 1978;(130):51–67.


33. Hernigou P, Flouzat-Lachaniette CH, Roussignol X, Poignard A. The natural progression of shoulder osteonecrosis related to corticosteroid treatment. Clin Orthop Relat Res 2010;468:1809–16.

34. Milner PF, Kraus AP, Sebes JI, et al. Osteonecrosis of the humer¬al head in sickle cell disease. Clin Orthop Relat Res 1993;(289):136–43.


35. da Silva Junior GB, Daher Ede F, da Rocha FA. Osteoarticular involvement in sickle cell disease. Rev Bras Hematol Hemoter 2012;34:156–64.



36. Mont MA, Payman RK, Laporte DM, Petri M, Jones LC, Hun¬gerford DS. Atraumatic osteonecrosis of the humeral head. J Rheumatol 2000;27:1766–73.

37. Orlić D, Jovanović S, Anticević D, Zecević J. Frequency of idio¬pathic aseptic necrosis in medically treated alcoholics. Int Or¬thop 1990;14:383–6.

39. Gerster JC, Camus JP, Chave JP, Koeger AC, Rappoport G. Mul¬tiple site avascular necrosis in HIV infected patients. J Rheuma¬tol 1991;18:300–2.
40. Attarian DE. Multifocal osteonecrosis and human immunodefi¬ciency virus infection. J South Orthop Assoc 2002;11:172–3.

41. Verbon A, Prins JM. Shoulder pain in two HIV-seropositive pa¬tients: avascular necrosis (AVN) of the bone. Neth J Med 2010;68:322–5.

43. Slichter SJ, Stegall P, Smith K, Huang TW, Harker LA. Dysbaric osteonecrosis: a consequence of intravascular bubble formation, endothelial damage, and platelet thrombosis. J Lab Clin Med 1981;98:568–90.

44. Colegate-Stone TJ, Aggarwal S, Karuppaiah K, Tavakkolizadeh A, Sinha J, Reichert IL. The staged management of gleno-hu¬meral joint osteonecrosis in patients with haematological-in-duced disease: a cohort review. Int Orthop 2018;42:1651–9.


45. Ficat RP. Idiopathic bone necrosis of the femoral head: early di¬agnosis and treatment. J Bone Joint Surg Br 1985;67:3–9.


46. Dines JS, Strauss EJ, Fealy S, Craig EV. Arthroscopic-assisted core decompression of the humeral head. Arthroscopy 2007;23:103e1-4.

47. Steffensmeier AM, Kirkham K, Wiemann JM. Core decompres¬sion with synthetic grafting as a joint preservation strategy in humeral avascular necrosis due to sickle cell anemia: a case re¬port. J Orthop Case Rep 2016;6:62–4.
48. Makihara T, Yoshioka T, Sugaya H, Yamazaki M, Mishima H. Autologous concentrated bone marrow grafting for the treat¬ment of osteonecrosis of the humeral head: a report of five shoulders in four cases. Case Rep Orthop 2017;2017:4898057.



49. Galloway MR, Horodyski M, Wright TW. Arthroscopically as¬sisted fibular strut allograft for treatment of osteonecrosis of proximal humerus. J Surg Orthop Adv 2013;22:277–82.


50. Zlotolow DA, Catalano LW 3rd, Barron OA, Glickel SZ. Surgical exposures of the humerus. J Am Acad Orthop Surg 2006;14:754–65.


51. Mont MA, Ragland PS, Etienne G. Core decompression of the femoral head for osteonecrosis using percutaneous multiple small-diameter drilling. Clin Orthop Relat Res 2004;(429):131–8.

52. Gerber C, Schneeberger AG, Vinh TS. The arterial vasculariza¬tion of the humeral head: an anatomical study. J Bone Joint Surg Am 1990;72:1486–94.


53. Chapman C, Mattern C, Levine WN. Arthroscopically assisted core decompression of the proximal humerus for avascular ne¬crosis. Arthroscopy 2004;20:1003–6.


54. Liu ZH, Guo WS, Li ZR, et al. Porous tantalum rods for treating osteonecrosis of the femoral head. Genet Mol Res 2014;13:8342–52.


55. Nadeau M, Séguin C, Theodoropoulos JS, Harvey EJ. Short term clinical outcome of a porous tantalum implant for the treatment of advanced osteonecrosis of the femoral head. Mcgill J Med 2007;10:4–10.



56. Zhang Y, Li L, Shi ZJ, Wang J, Li ZH. Porous tantalum rod im¬plant is an effective and safe choice for early-stage femoral head necrosis: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol 2013;23:211–7.


57. Li X, Xu X, Wu W. Comparison of bone marrow mesenchymal stem cells and core decompression in treatment of osteonecro¬sis of the femoral head: a meta-analysis. Int J Clin Exp Pathol 2014;7:5024–30.


58. Civinini R, De Biase P, Carulli C, et al. The use of an injectable calcium sulphate/calcium phosphate bioceramic in the treat¬ment of osteonecrosis of the femoral head. Int Orthop 2012;36:1583–8.



59. Sionek A, Czwojdziński A, Ko walczewski J, et al. Hip osteone¬croses treated with calcium sulfate-calcium phosphate bone graft substitute have different results according to the cause of osteonecrosis: alcohol abuse or corticosteroid-induced. Int Or¬thop 2018;42:1491–8.

60. Luo Y, Li D, Xie X, Kang P. Porous, lithium-doped calcium poly¬phosphate composite scaffolds containing vascular endothelial growth factor (VEGF)-loaded gelatin microspheres for treating glucocorticoid-induced osteonecrosis of the femoral head. Biomed Mater 2019;14:035013.


61. Yu PA, Peng KT, Huang TW, Hsu RW, Hsu WH, Lee MS. Inject¬able synthetic bone graft substitute combined with core decom¬pression in the treatment of advanced osteonecrosis of the fem¬oral head: a 5-year follow-up. Biomed J 2015;38:257–61.


62. Chang CH, Liao TC, Hsu YM, Fang HW, Chen CC, Lin FH. A poly(propylene fumarate)--calcium phosphate based angiogen¬ic injectable bone cement for femoral head osteonecrosis. Biomaterials 2010;31:4048–55.


63. Zhao P, Hao J. Analysis of the long-term efficacy of core decom¬pression with synthetic calcium-sulfate bone grafting on non-traumatic osteonecrosis of the femoral head. Med Sci (Par¬is) 2018;34:43–6.

64. Jiang HJ, Huang XJ, Tan YC, Liu DZ, Wang L. Core decompres¬sion and implantation of calcium phosphate cement/Danshen drug delivery system for treating ischemic necrosis of femoral head at Stages I, II and III of antigen reactive cell opsonization. Chin J Traumatol 2009;12:285–90.

65. Evaniew N, Tan V, Parasu N, et al. Use of a calcium sulfate-calci¬um phosphate synthetic bone graft composite in the surgical management of primary bone tumors. Orthopedics 2013;36:e216–22.


66. Yashavantha Kumar C, Nalini KB, Menon J, Patro DK, Banerji BH. Calcium sulfate as bone graft substitute in the treatment of osseous bone defects, a prospective study. J Clin Diagn Res 2013;7:2926–8.