|
 |
- Search
| Clin Shoulder Elb > Volume 23(2); 2020 > Article |
|
Abstract
Background
Methods
Results
Conclusions
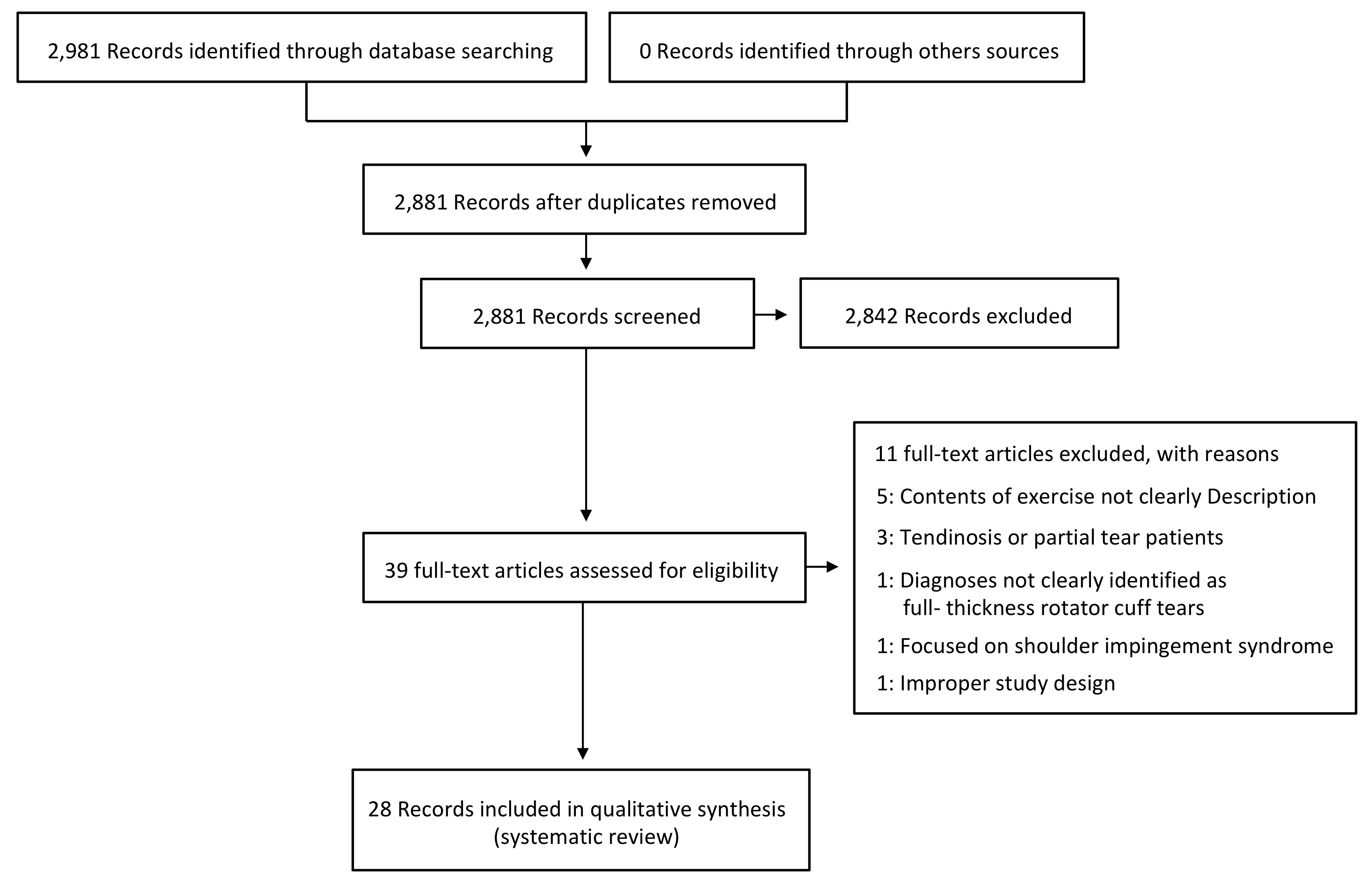
Fig.ô 2.
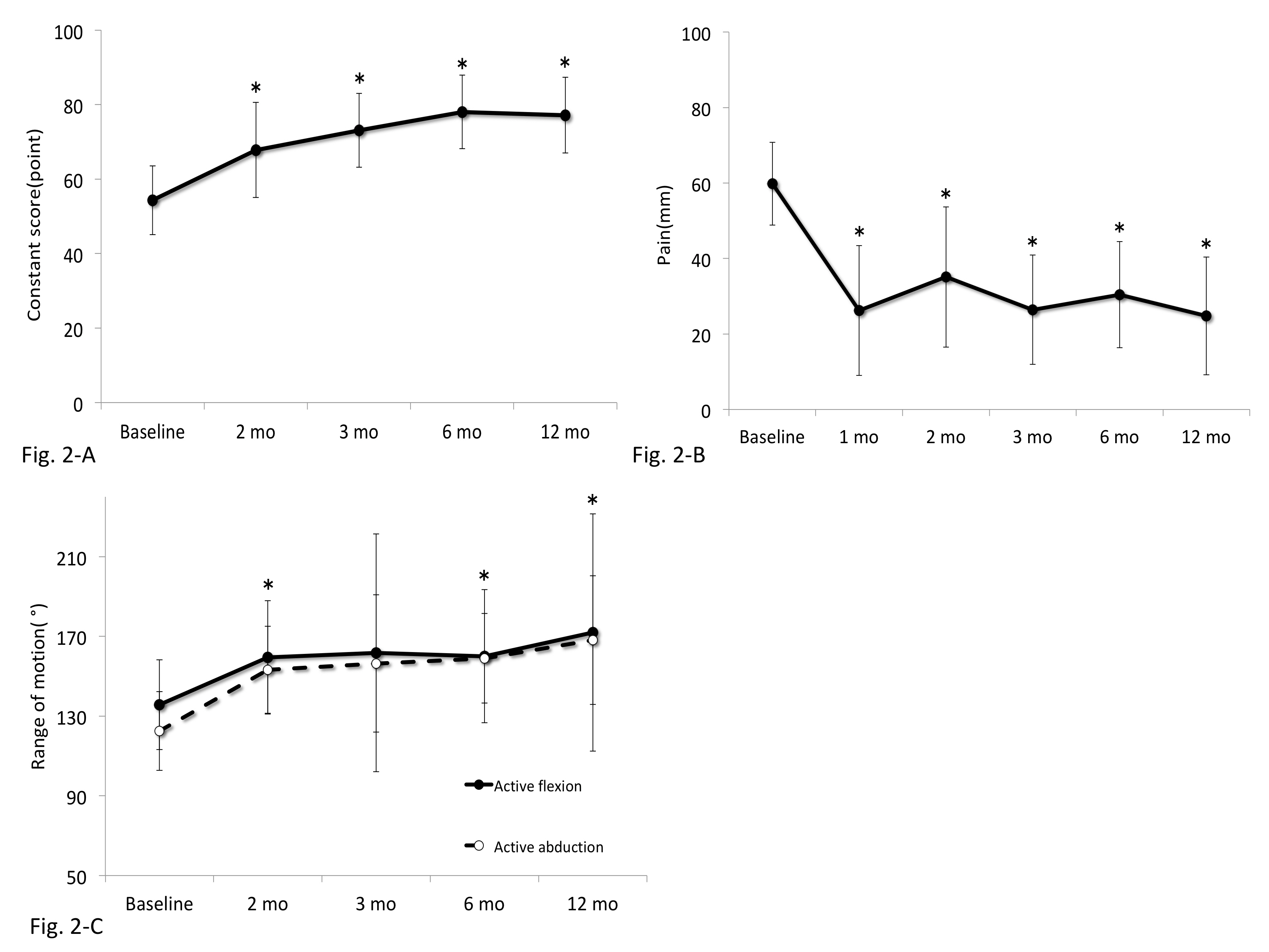
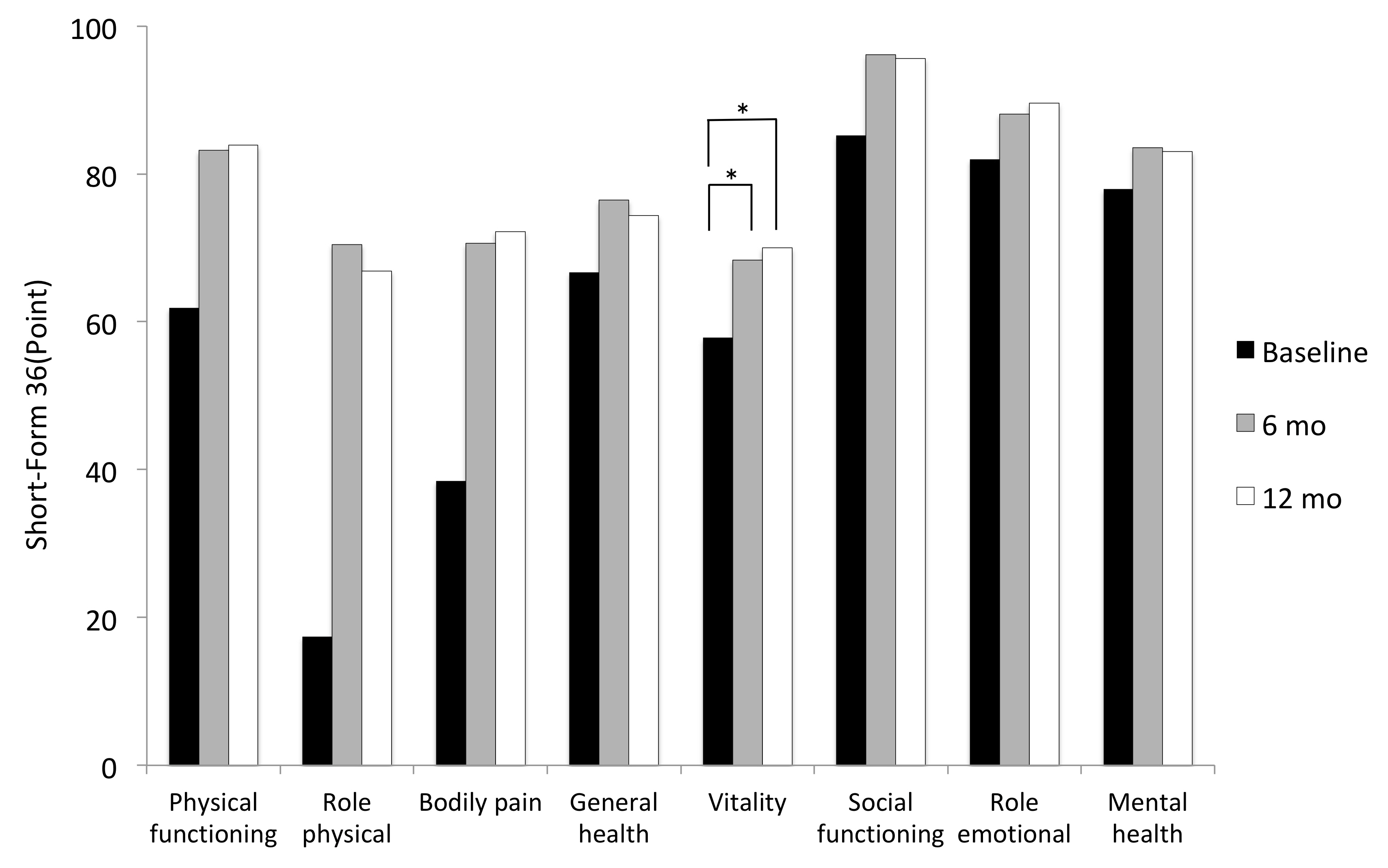
Fig.ô 3.
Tableô 1.
| Study | Type of study | Subject (n) | Sample size | Mean age (yr) | Sex (M:F) | Outcome measure | Follow-up |
|---|---|---|---|---|---|---|---|
| Mischke et al. (2016) [6] | Case report | Nonoperative (1) | 1 | 57 | F, 1 | Pain (VAS), quick | Visit, 13 |
| DASH, GROC, ROM | |||||||
| Miller et al. (2016) [7] | Case series | Nonoperative (5) | 5 | 60.2 | 2:3 | ASES, WORC, DASH, strength | 3 mo |
| Baumer et al. (2016) [8] | Cohort study | Physical therapy (25) | 25 | 60.2 | 7:18 | Pain (VAS), WORC, strength, ROM | 8 wk |
| Healthy controls (25) | 25 | 59 | 7:18 | ||||
| Lambers Heerspink et al. (2015) [9] | RCT | Conservative (31) | 31 | 60.5 | 20:11 | Pain (VAS), disability (VAS), CS, DSST | 1 yr |
| Surgery (25) | 25 | 60.8 | 15:10 | ||||
| Kukkonen et al. (2015) [10] | RCT | Physiotherapy (55) | 55 | 64 | 24:31 | CS, pain (VAS) | 2 yr |
| Acromioplasty and physiotherapy (57) | 57 | 65 | 29:28 | ||||
| Repair, acromioplasty, and physiotherapy (55) | 55 | 65 | 29:26 | ||||
| Collin et al. (2015) [11] | Case series | Nonoperative (45) | 45 | 67 | 17:28 | ROM, CS | 2 yr |
| Nejati et al. (2014) [12] | Case report | Nonoperative (1) | 1 | 53 | M, 1 | Pain (VAS), ROM | 6 mo |
| Boorman et al. (2014) [13] | Case series | 3-Month supervised program of nonoperative | 93 | 60 | 54:39 | RC-QOL, ROM, strength | 3 mo |
| ãSuccessful (no surgery)ã (70) | |||||||
| ãFailed (underwent surgery)ã (23) | |||||||
| Benazzo et al. (2014) [14] | Case report | Nonoperative (1) | 1 | 23 | F, 1 | SST, CS, ROM, strength | 29 mo |
| Kuhn et al. (2013) [15] | Cohort study | Physiotherapy (422) | 422 | 62.6 | 206:194 | SF-12, ASES, WORC, SANE, Shoulder Activity Scale | 2 yr |
| Krischak et al.(2013) [16] | RCT | Occupational therapy (22) | 38 | 55.3 | 24:14 | Pain (VAS), EQ-5D, strength, ROM, CS | 2 mo |
| Home-based exercises (16) | |||||||
| Kijima et al. (2012) [17] | Case series | Nonoperative (43) | 43 | 62 | 30:13 | JOAS | 12 yr |
| Gialanella et al. (2011) [3] | RCT | Physiotherapyÿ¥corticosteroids (û1) (20) | 60 | 78.7 | 2:18 | Pain (VAS), shoulder functional status, CS | 6 mo |
| Physiotherapyÿ¥corticosteroids (û2) (20) | 77.3 | 1:19 | |||||
| Physiotherapy (20) | 79.4 | 2:18 | |||||
| Tanaka et al. (2010) [18] | Case series | Conservative (128) | 128 | 69 | 67:61 | CS, night pain, ROM | 3.7 mo |
| Moosmayer et al. (2010) [19] | RCT | Nonoperative (51) | 51 | 61 | 36:15 | CS, ASES, SF-36, pain (VAS), ROM, strength, satisfaction | 1 yr |
| Operative (52) | 52 | 59 | 37:15 | ||||
| Baydar et al. (2009) [20] | Case series | Nonoperative (20) | 20 | 60.9 | 7:13 | ROM, ASES, CS, SF-36, strength | 6 mo |
| Levy et al. (2008) [21] | Case series | Nonoperative (17) | 17 | 80 | 6:11 | Strength, CS | 9 mo |
| KoubûÂa et al. (2006) [22] | Case series | Conservative (24) | 24 | 59.2 | 9:15 | CS, pain (VAS), impairment | 6 mo |
| Ainsworth (2006) [23] | Case series | Nonoperative (10) | 10 | 76 | 4:6 | OSDQ, SF-36 | 3 mo |
| Heers et al. (2005) [24] | Case series | Nonoperative (34) | 34 | 60.4 | 13:23 | CS, ROM | 3 mo |
| Vad et al. (2002) [25] | Cohort study | G1a: physiotherapy+medication (28) | 108 | G1:63.2 | 50:58 | SRQ, ROM, strength | 3.2 yr |
| G1b: physiotherapy+medication+steroid (12) | G2:62.9 | ||||||
| G2: arthroscopic (failed G1a/1b) (32) | G3:59.4 | ||||||
| G3: primary surgical repair (36) | |||||||
| Shibata et al. (2001) [26] | RCT | G1: sodium hyaluronate (38) | 78 | G1:59.5 | 55:23 | UCLA, ROM, satisfaction | 24 wk |
| G2: Steroid (40) | G2:60.4 | ||||||
| Goldberg et al. (2001) [27] | Case series | Nonoperative (46) | 46 | 65 | 22:24 | SST, SF-36 | 2.5 yr |
| Yamada et al. (2000) [28] | Case series | Nonoperative (14) | 14 | 70 | 9:5 | JOAS | 4 yr |
| Operative (26) | 26 | 62 | 24:2 | ||||
| Wirth et al. (1997) [29] | Case series | Nonoperative (60) | 60 | 64 | 38:22 | ASES | 2 yr |
| Hawkins et al. (1995) [30] | Case series | Nonoperative (33) | 33 | 59.6 | 27:6 | CS, ASES | 3.8 yr (2.6ã4.6) |
| Bokor et al. (1993) [31] | Case series | Nonoperative (53) | 53 | 62.2 | 40:13 | ASES, UCLA, ROM | 7.6 yr |
| (3.7ã12) | |||||||
| Itoi et al. (1992) [32] | Case series | Nonoperative (124) | 124 | 63 | 59:55 | MWC, ROM, strength | 3.4 yr (1ã9) |
VAS, visual analog scale; DASH, Disabilities of the Arm, Shoulder, and Hand; GROC, global rating of change; ROM, range of motion; ASES, American Shoulder and Elbow Surgeons; WORC, Western Ontario Rotator Cuff index; RCT, randomized controlled trial; CS, Constant score; DSST, Dutch Simple Shoulder Test; RC-QOL, Rotator Cuff Quality-of-Life Index; SST, Simple Shoulder Test; SF-12, short-form 12 questionnaires; SANE, Single Assessment Numeric Evaluation; EQ-5D, EuroQol questionnaire; JOAS, Japanese orthopedic association score; SF-36, G, group; short form 36 questionnaires; OSDQ, Oxford Shoulder Disability Questionnaire; SRQ, shoulder rating questionnaire; UCLA, University of California at Los Angeles Shoulder Score; MWC, modified Wolfgangãs criteria.
REFERENCES
- TOOLS
-
METRICS

-
- 10 Crossref
- 25,153 View
- 264 Download
- Related articles in Clin Should Elbow
-
Patch augmentation in patients with large to massive rotator cuff tear2023 March;26(1)
Bilateral acromial stress fractures in a patient with a massive rotator cuff tear2020 June;23(2)