Evaluation of Muscular Atrophy and Fatty Infiltration Using Time-zero Magnetic Resonance Imaging as Baseline Data, After Rotator Cuff Repair
Article information
Abstract
Background
This study evaluated postoperative changes in the supraspinatus from time-zero to 6 months, using magnetic resonance imaging (MRI). We hypothesized that restoration of the musculotendinous unit of the rotator cuff by tendon repair immediately improves the rotator cuff muscle status, and maintains it months after surgery.
Methods
Totally, 76 patients (29 men, 47 women) with rotator cuff tears involving the supraspinatus tendon who underwent arthroscopic rotator cuff repairs were examined. MRI evaluation showed complete repair with intact integrity of the torn tendon at both time-zero and at 6 months follow-up. All patients underwent standardized MRI at our institution preoperatively, at 1 or 2 days postoperative, and at 6 months after surgery. Supraspinatus muscular (SSP) atrophy (Thomazeau grade) and fatty infiltrations (Goutallier stage) were evaluated by MRI. The cross-sectional area of SSP in the fossa was also measured.
Results
As determined by MRI, the cross-sectional area of SSP significantly decreased 11.41% from time-zero (immediate repair) to 6 months post-surgery, whereas the Goutallier stage and Thomazeau grade showed no significant changes (p < 0.01). Furthermore, compared to the preoperative MRI, the postoperative MRI at 6 months showed a no statistically significant increase of 8.03% in the cross-sectional area. In addition, morphological improvements were observed in patients with high grade Goutallier and Thomazeau at time-zero, whereas morphology of patients with low grade factors were almost similar to before surgery.
Conclusions
Our results indicate that cross-sectional area of the initial repair appears to decrease after a few months postoperatively, possibly due to medial retraction or strained muscle.
Introduction
Tendon tear of the rotator cuff alters the muscular structure. Over time, the musculotendinous units of the torn tendon retract and the muscle undergoes atrophy, fatty infiltration, and fibrosis, with loss of contractility and elasticity [1,2]. Muscular atrophy and fatty infiltration are recognized as important characteristics of rotator cuff tendon tear. They are associated with the severity and chronicity of the tendon tear [1], resulting in decreased optimal repair [3], inferior clinical outcome, and higher re-tear rate [4]. More recently, muscular atrophy and fatty infiltration are indicated as important prognostic factors in the anatomical and functional outcomes of rotator cuff repairs [1,3-6].
Regression or progression of muscular atrophy and fatty infiltration after cuff repair has gained momentum as a debatable issue. Some researchers suggest that muscle status can be improved after successful rotator cuff repair [5-8], whereas others argue there is no improvement of muscle status despite complete and successful repair [4,9,10]. To address this issue in the clinical setting, past studies have compared preoperative computed tomography (CT) images or magnetic resonance imaging (MRI) with postoperative images at several months or years after repair.
However, previous results have an inherent limitation: the retraction of a tear can alter the comparability among different MRI scans [11]. Repairing a torn tendon acutely restores the musculotendinous unit of the rotator cuff [5-7,11]. This immediate change in muscle status after repair and subsequent healing process may preclude direct comparison of the muscle status between preoperative and postoperative MRIs months or years after surgery. Although recent literature shows that reversal could occur from 6 months to 2 years, the postoperative period from time-zero to 6 months has not been studied previously [12]. Furthermore, it remains to be determined if the initial repair can withstand the 6 months early rehabilitation period, or if there is a change in repair integrity.
This study was therefore undertaken to evaluate the postoperative changes in the supraspinatus muscle from time-zero to 6 months. We hypothesized that restoration of the musculotendinous unit of the rotator cuff by tendon repair would improve the rotator cuff muscle status immediately after surgery, and maintain it months after surgery.
Methods
Patient Selection
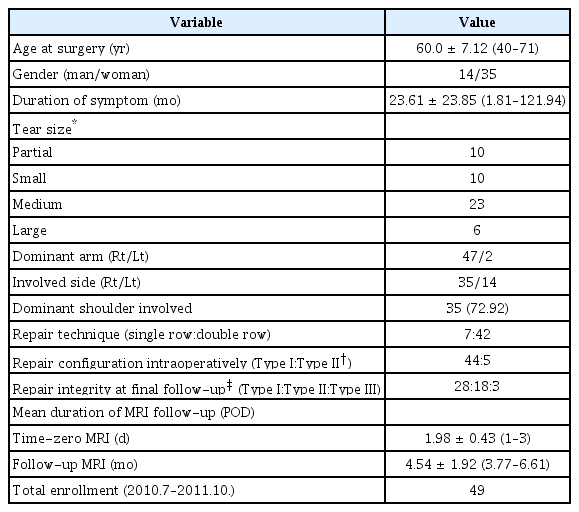
From July 2010 to October 2011, 76 patients who underwent arthroscopic rotator cuff repair for degenerative rotator cuff tears were enrolled in this study. Patients with partial- and full-thickness rotator cuff tears involving the supraspinatus tendon, such as isolated supraspinatus tears or supraspinatus, infraspinatus, and/or subscapularis tears, were included. All patients underwent three MRI assessments at Samsung Medical Center: preoperatively, 1 day or 2 days after surgery, and at 6 months (mean) after surgery. Complete repair was achieved in all the enrolled cases: type I complete repair with the tendon mobilized to the far lateral end of the greater tuberosity covering nearly the entire original footprint, and type II complete repair, with less optimal coverage of the entire medial-lateral footprint, indicating that the tendon is mobilized and attached to less than half of the medial side of the greater tuberosity [3]. Following cases were excluded from the final analysis: re-tear, isolated subscapularis tear, calcific tendinitis, missing Y-view image on T2 sagittal oblique MRIs, partial repairs (type III or IV repair [3]), patients who underwent latissimus dorsi transfer, and patients lacking either time-zero and/or 6-month follow-up MRI. Also excluded were patients with infection, revision, or concomitant systemic disease such as rheumatoid arthritis and systemic lupus erythematosus. The final study cohort comprised of 49 patients. This study was approved by Samsung Medical Center Institutional Review Board (No. SMC: 2016-02-019).
Magnetic Resonance Imaging Examination
The 49 patients included in the study were examined preoperatively with MRI or magnetic resonance arthrography (MRA): 12 patients underwent non-contrast MRI, and 37 patients underwent indirect MRA. Based on the MRI protocol, patients admitted a day before the surgery underwent indirect MRA whereas outpatients underwent non-contrast MRI during the study period at our hospital. Recent literature has reported that indirect MRA is likely to produce a similar outcome as non-contrast MRI when diagnosing for supraspinatus and infraspinatus muscle tears, except for partial articular supraspinatus tendon avulsion lesion [13]. Since our study evaluated only the supraspinatus, we expected that the 2 different MRI methods would not influence our results. All patients underwent non-contrast MRI for time-zero and 6-month follow-up. Non-contrast MRI was performed with a 3.0-T magnetic resonance imager (Gyroscan Intera Achieva; Philips Medical Systems, Best, The Netherlands) with a dedicated receive-only shoulder coil. Patients were imaged supine, with the humerus in a neutral position and the thumb pointing upward. For MRA, 0.1 mmol/kg of gadobutrol (Gadovist; Bayer Healthcare, Berlin, Germany) was injected into an antecubital vein. Immediately after injecting the contrast media, patients were instructed to exercise their shoulders for 15 minutes, followed by MRI being performed similar to the non-contrast MRI. Conventional two-dimensional MRIs were obtained with fat-suppressed T1-weighted fast spin echo sequences in the axial and oblique coronal planes parallel to the long axis of the supraspinatus tendon, and oblique sagittal plane perpendicular to the long axis of the supraspinatus tendon (3-mm thick; 1-mm gap between slices; field of view, 15 cm; matrix size of 224 pixels [224×224]; echo train length, 16). All measurements were performed on a picture archiving and communication system (PACS) monitor (GE Healthcare Integrated IT Solutions, Barrington, IL, USA) using a mouse-point cursor and automated computer calculation for distance and angle (Fig. 1).
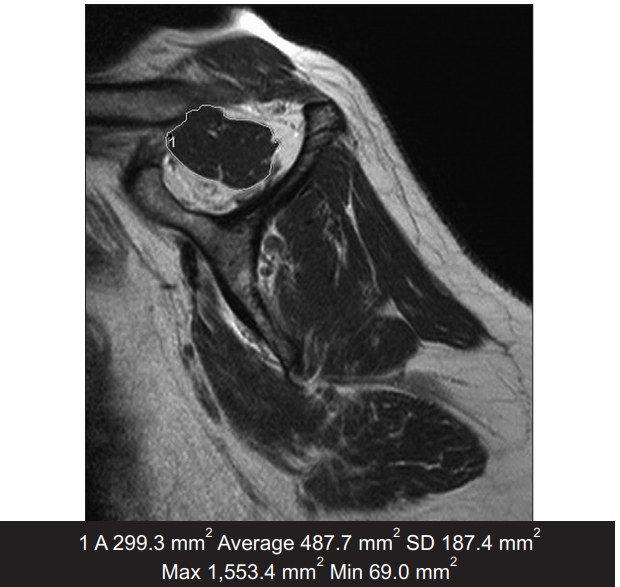
The area was measured using the Centricity-Radiology RA1000 workstation (GE Healthcare Integrated IT Solutions, Barrington, IL, USA) by use of a mouse-point cursor and automated computer calculation for distance and angle. All measurements were performed twice by 2 independent observers. SD: standard deviation, Max: maximum, Min: minimum.
Magnetic Resonance Imaging Evaluation
The results were evaluated by 2 independent orthopedic surgeons, blinded to each other to increase interobserver reliability. The Goutallier stage, Thomazeau grade, and occupation ratio of the supraspinatus were individually measured using the same image cuts. For intraobserver reliability, measurements were done at a 2-week interval period. The complete footprint coverage of the supraspinatus tendon was first assessed on a T2-weighted coronal plane at time-zero MRI in all patients. This was followed by assessing the tendon integrity on a T2-weighted coronal plane in the 6 months postoperative MRI using the Sugaya classification [14].
1) Fatty infiltration measured using the Goutallier stage
Goutallier stages are classified as: stage 0, no fat; stage 1, some fatty streaks; stage 2, less fat than muscle; stage 3, equal amounts of fat and muscle; stage 4, more fat than muscle [1,15]. For statistical analysis, each stage was given a score. Although originally described for CT, previous studies have appropriately applied this classification system to MRI [10].
2) Muscular atrophy measured using the Thomazeau grade
The Thomazeau grade is based on the occupation ratio of the supraspinatus with the supraspinatus fossa: grade 1, 0.6–1.0 (normal/slight); grade 2, 0.4–0.6 (moderate); grade 3, <0.4 (severe) [8]. Atrophy of the supraspinatus was graded as 1, 2, and 3. For statistical analysis, normal and slight were given a score of 1; moderate, 2; and severe, 3.
3) Muscle atrophy measured using cross-sectional area
The cross-sectional area of the supraspinatus muscle in the supraspinatus fossa was measured using the freehand ‘polygonal region of interest’ tool on the PACS workstation. The T2-weighted, sagittal oblique plane images of the point where the coracoids and the scapular spine meet the scapular body were used for all evaluations.
Clinical Evaluation
All patients were clinically evaluated via the pain visual analogue scale (PVAS), function visual analogue scale (FVAS), American Shoulder and Elbow Surgeons (ASES) score [12], and Constant score [16]. Clinical evaluation was performed a day before surgery, approximately 6 months after surgery, approximately 1 year after surgery, and at final follow-up (mean, 4 years). Those who were unable to visit the out-patient clinic had a telephone survey at the final follow-up. Clinical scoring was performed by a physiotherapist blinded to the study design or the clinical results.
Operative Technique
All surgeries were performed by a single senior surgeon (JCY). Patients were operated in a semi-lateral decubitus position and were administered regional anesthesia. Torn tendons were systematically identified, recorded, mobilized, and reattached to the greater tuberosity using suture anchors with a simple stitch, in a single-row fashion in 7 shoulders and double-row fashion with a suture bridge in 42 shoulders. Complete coverage of the rotator cuff footprint was achieved in all patients. Type I repair was performed in 44 shoulders and type II in 5 shoulders. All patients underwent a routine rehabilitation protocol, with immobilization for 4 weeks followed by active-assisted passive range of motion (ROM) exercises. Patients were subjected to stretching and active strengthening exercise after achieving full ROM.
Statistical Analysis
Continuous variables, including preoperative and postoperative clinical scores (PVAS, FVAS, ASES, and Constant score), were compared by analysis of variance (ANOVA). Changes in fatty infiltration, muscle atrophy, and cross-sectional area of the supraspinatus muscle between serial MRI studies were evaluated by repeated ANOVA using the SAS ver. 9.3 (SAS Institute, Cary, NC, USA). Interclass correlation coefficients between the 2 independent observers were analyzed by applying IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). p-values were corrected by Bonferroni method in case of multiple testing, and considered significant less than 0.05.
Results
Interobserver and intraobserver reliability were excellent for all factors evaluated (Table 1). In all patients, complete footprint coverage of the supraspinatus tendon was confirmed on T2-weighted, coronal-plane MRI at time-zero, suggesting that the musculotendinous unit of the supraspinatus was successfully restored. Furthermore, Sugaya classification [14] confirmed the integrity of the repaired tendons on T2-weighted, coronal-plane MRI at postoperative 6 months. The baseline characteristics of the patients in our study are presented in Table 2 [3,14,17].
Clinical Outcome
Significant improvements were observed in the PVAS, FVAS, ASES, and Constant scores from preoperative to postoperative 6 months, from 6 months to 1 year, and from preoperative to the final follow-up evaluations (Fig. 2).
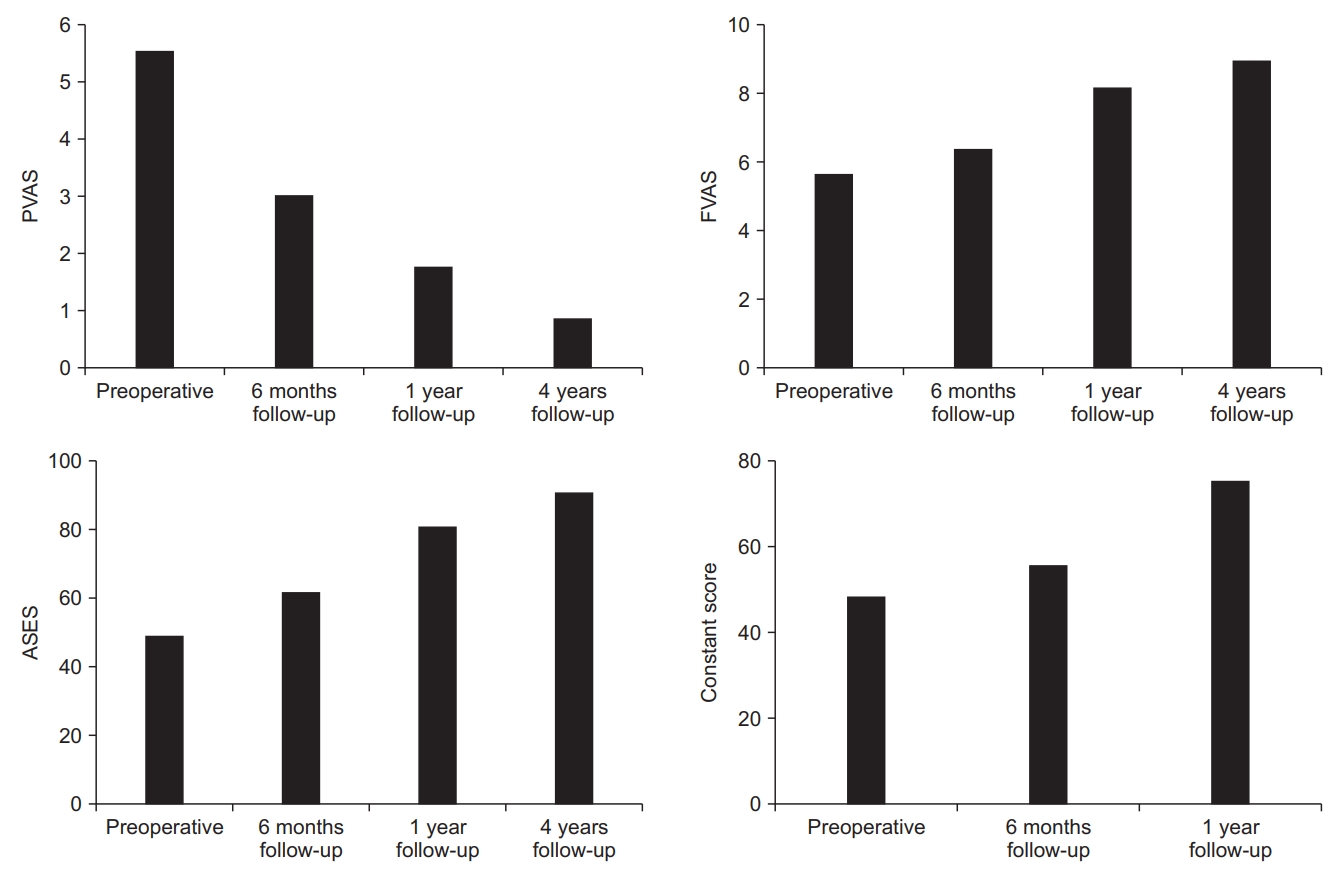
The pain visual analogue scale (PVAS), function visual analogue scale (FVAS), and American Shoulder and Elbow Surgeons (ASES) were significantly improved from preoperative to postoperative 6 months (p<0.001), from 6 months to 1 year (p<0.001), and from preoperative to the final follow-up evaluations (p<0.001). Constant scores were significantly improved from preoperative to postoperative 6 months (p<0.001), and from 6 months to 1 year (p<0.001).
Magnetic Resonance Imaging Evaluations
1) Fatty infiltration measured using the Goutallier stage
From preoperative to time-zero, a significant improvement was observed in the Goutallier stage of the supraspinatus (1.58–1.39, respectively; p=0.0034). However, no significant change was observed in the preoperative to 6-month follow-up MRI (1.58–1.30, respectively; p=0.06) or in the time-zero to 6-month follow-up MRI (1.39–1.30, p=0.93) (Fig. 3A). Notably, Goutallier stages 3 and 4 were significantly decreased after immediate rotator cuff repair (p<0.01). Furthermore, we observed an increase in the relative distribution of stage 2 (p=0.65), with no significant difference being observed for stage 0 and 1 (p=0.85) (Fig. 3B).
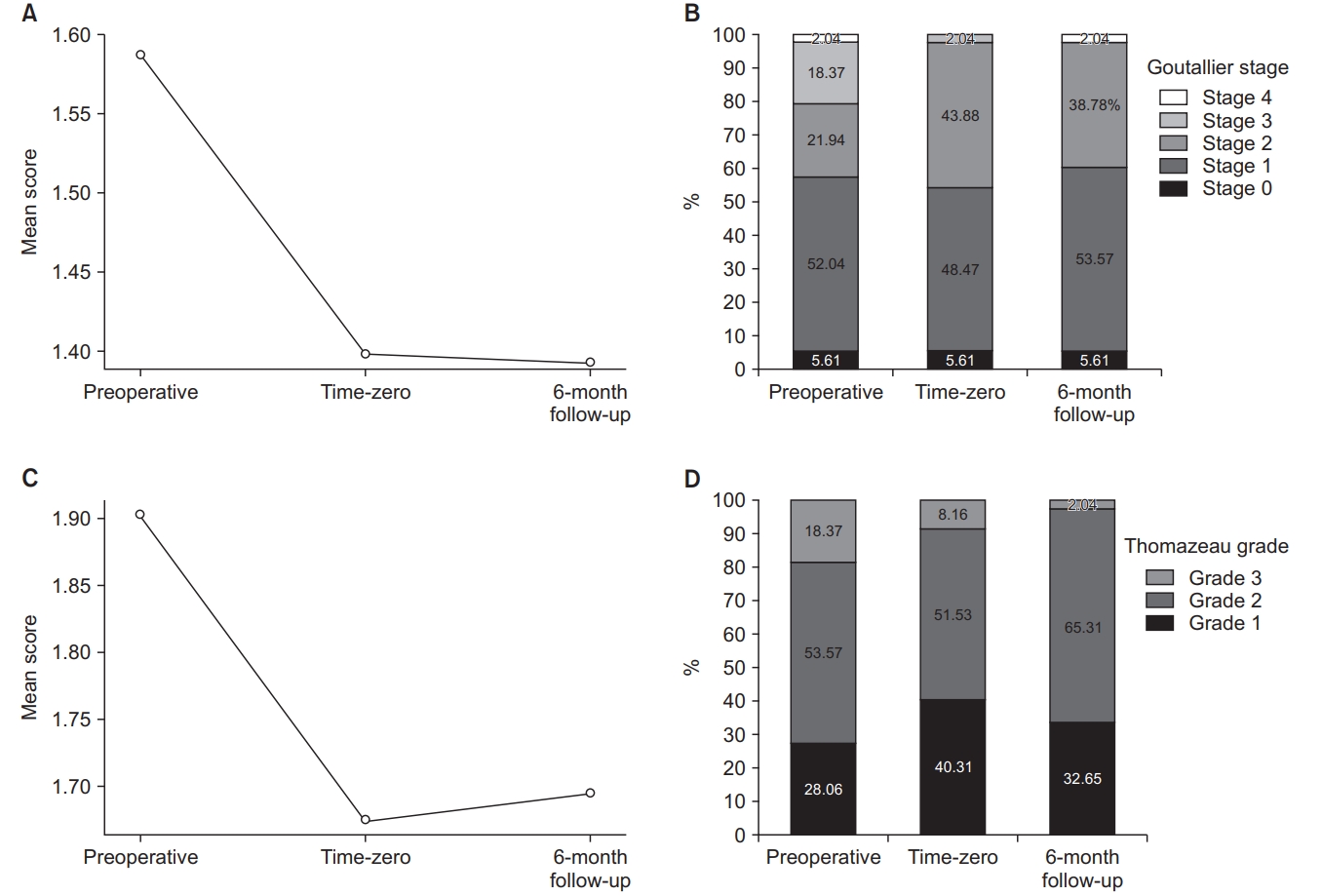
(A) Goutallier stages were significantly improved from preoperative magnetic resonance imaging (MRI) to time-zero MRI (p=0.0034). However, no significant changes were observed between preoperative to 6-month follow-up MRI (p=0.06), and time-zero to 6-month follow-up MRI (p=0.93). (B) Goutallier stage 3 and 4 were significantly decreased from preoperative MRI to time-zero MRI (p<0.01). (C) Thomazeau grade were significantly improved from preoperative MRI to time-zero MRI (p=0.0015), although there were no significant differences between preoperative and follow-up MRI, and time-zero and follow-up MRI (p=0.60, p=0.67). (D) Thomazeau grades 3 were significantly decreased from preoperative MRI to time-zero MRI (p<0.01).
2) Muscle atrophy measured using the Thomazeau grade
After immediate repair, the mean atrophy grade significantly improved from 1.90 to 1.67 (p=0.0015), but no significant differences were noted between preoperative and 6-month follow-up, or between time-zero and 6-month follow-up (p=0.60 and p=0.67, respectively) (Fig. 3C). Immediately after rotator cuff repair, the number of patients with Thomazeau grade 3 muscle atrophy decreased significantly (p<0.01), whereas the number of patients with Thomazeau grades 1 and 2 remained unchanged (Fig. 3D).
3) Muscle atrophy measured using cross-sectional area
The mean cross-sectional area of the supraspinatus significantly improved from 373.76 mm2 preoperatively to 446.12 mm2 at time-zero (p<0.0001) (Fig. 4A). Immediately after surgery, the mean cross-sectional area increased to 21.72%. MRI revealed significantly reduced cross-sectional area from time-zero to 6 months follow-up (446.12 to 388.48 mm2, respectively; 11.41% reduction; p<0.0001). Comparison of preoperative MRI with 6-month MRI showed an 8.03% increase in the cross-sectional area, which was not statistically significant (p=0.14) (Fig. 4B-D).
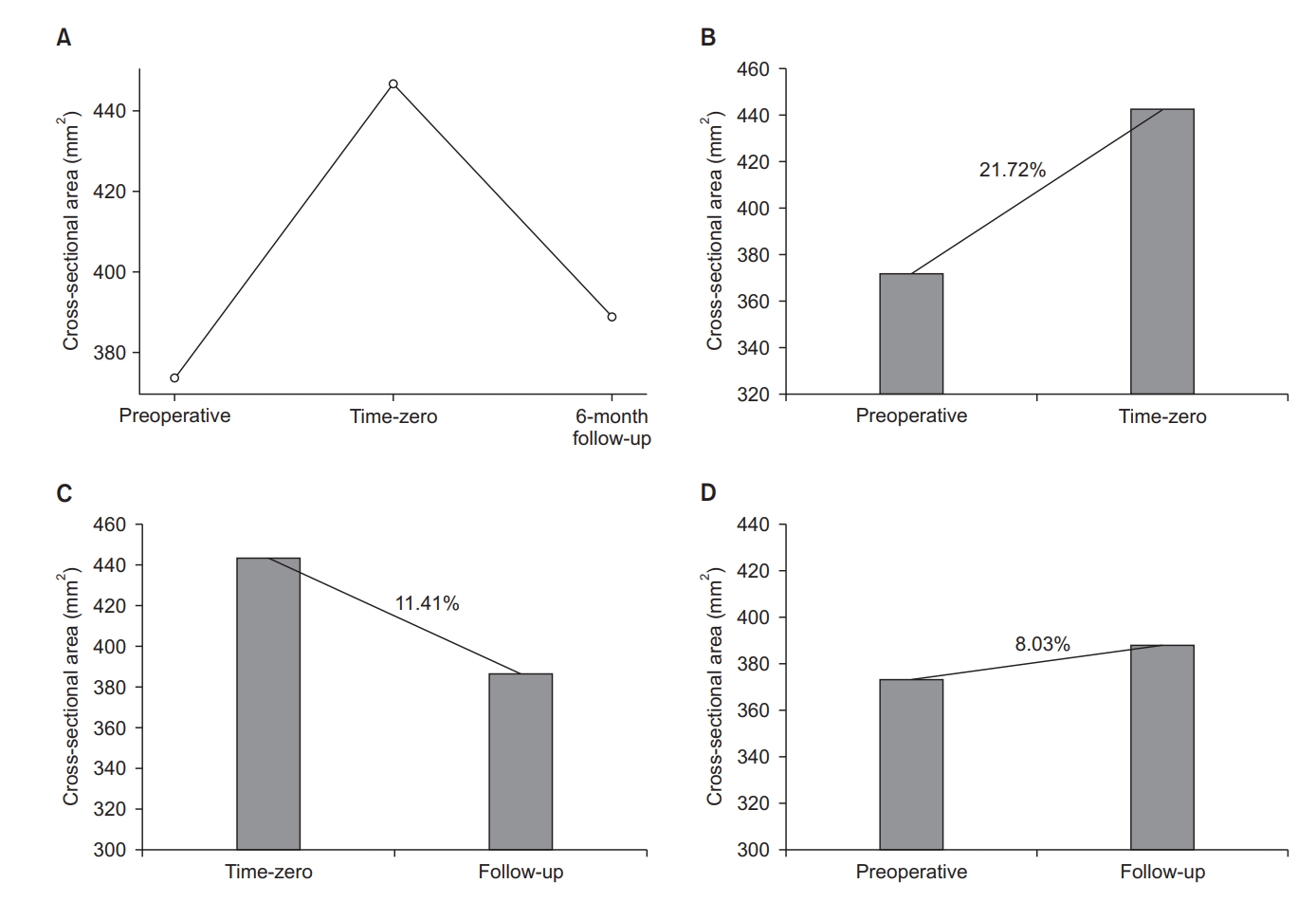
(A) Cross-sectional area of the supraspinatus significantly improved from 373.76 mm2 preoperatively to 444.12 mm2 time-zero magnetic resonance imaging (MRI) (p<0.0001). Cross sectional area of supraspinatus changes were: (B) increased 21.72% from preoperative MRI to time-zero MRI (p<0.0001), (C) decreased 11.41% from time-zero MRI to follow-up MRI (p<0.0001), and (D) increased 8.03% from preoperative to follow-up MRI, although difference was statistically not significant (p=0.14).
Discussion
This study was undertaken to evaluate changes in the morphology of fatty infiltration and muscle atrophy of rotator cuff muscles after arthroscopic rotator cuff repair by applying MRI. Our MRI results revealed 11.41% decrease in the cross-sectional area of the supraspinatus muscle from time-zero (immediate repair) to postoperative 6 months, but no significant changes were observed in the Goutallier stage and Thomazeau grades. Compared with preoperative MRI, the postoperative MRI at 6 months (mean) shows only an 8.03% increase in the cross-sectional area, which is statistically not significant. In addition, patients with high grade Goutallier and Thomazeau showed significant morphologic improvements at time-zero, whereas patients with low grade were almost similar to the pre-operative morphology.
Rotator cuff tear repair consistently results in decreased pain and increased shoulder function. However, the effects of repair on atrophy and fatty infiltration are still controversial [1,5,8,9,15]. Several studies using MRI have documented muscle atrophy reversal. Thomazeau et al. [8] observed that supraspinatus muscle atrophy improved in 18 of 22 rotator cuffs at 21 months after surgery, using a scoring system based on MRI signal intensities [18,19]. Gerber et al. [7] showed an insignificant increase in the cross-sectional area of the successfully repaired supraspinatus at 2 years, and concluded that atrophy may be reversed with successful repair. Goutallier et al. [20] found that at 18 months after successful repair, supraspinatus fatty infiltration was decreased in 6 of the 14 patients evaluated. Results of the current study suggest that even with grade 3 or 4 fatty infiltration, repair could result in improving the amount of atrophy and fat in the muscle. In an experimental study with rabbit models, Rubino et al. [5] reported that repair prevents further progression and atrophy of the rotator cuff.
Contrarily, Gladstone et al. [9] reported that at a minimum of 1 year, successful repair resulted in no morphologic improvement or reversal of muscle atrophy and fatty infiltration. Studies by Matsumoto et al. [18] and Shimizu et al. [19] showed no reversal of fatty infiltration at 6 and 12 months, respectively, after rotator cuff repair. However, these findings of atrophy reversal have an inherent limitation, as they were based on the comparison between preoperative and postoperative findings several months after repair, and the follow-up period was relatively short. Furthermore, these studies did not have baseline measurement after immediate repair and were instead compared with the preoperative muscle status.
Jo and Shin [11] investigated the changes in fatty infiltration and muscle atrophy by comparing preoperative MRI with time-zero MRI in 101 patients who underwent arthroscopic rotator cuff repair. They reported immediate improvement of fatty infiltration and rotator cuff atrophy after successful surgery. This study suggested that time-zero MRI provides the baseline data, which are clinically important in comparing changes in the muscle status. This finding coincides with our study results. However, their study did not include a longer follow-up period, especially the subsequent changes in fatty infiltration and muscle atrophy [11].
In our study, we observed changes in the muscle status using time-zero MRI as baseline data. Before commencing our study, we hypothesized that rotator cuff repair would improve the muscle status and maintain it months after surgery. However, MRIs from time-zero to 6-month follow-up reveal a decrease in the cross-sectional area, whereas the Goutallier stage and Thomazeau grade remain unchanged. McCarron et al. [21] undertook CT assessment of tendon retraction in 14 patients who underwent arthroscopic rotator cuff repair using Tantalum markers placed within the repaired tendons. This study showed that at postoperative 6 weeks, the repaired tendon significantly retracted medially without tear. They suggested that the medial retraction of the repaired tendon might be a natural phenomenon in patients who underwent rotator cuff repair. Baring et al. [22] reported that retraction of repaired tendon occurs 4 weeks after rotator cuff repair. This phenomenon in our study might explain why the cross-sectional area decreases at 6 months, compared to the MRI findings at time-zero (Fig. 5). Another possible explanation for reduced cross-sectional area might be that postoperative immobilization and non-weight-loading exercises cause further atrophy of the repaired tendon. In addition, immediate postoperative MRI might show muscle edema due to saline infusion during the arthroscopic surgery, thereby resulting in overestimation of the cross-sectional area at time-zero MRI.
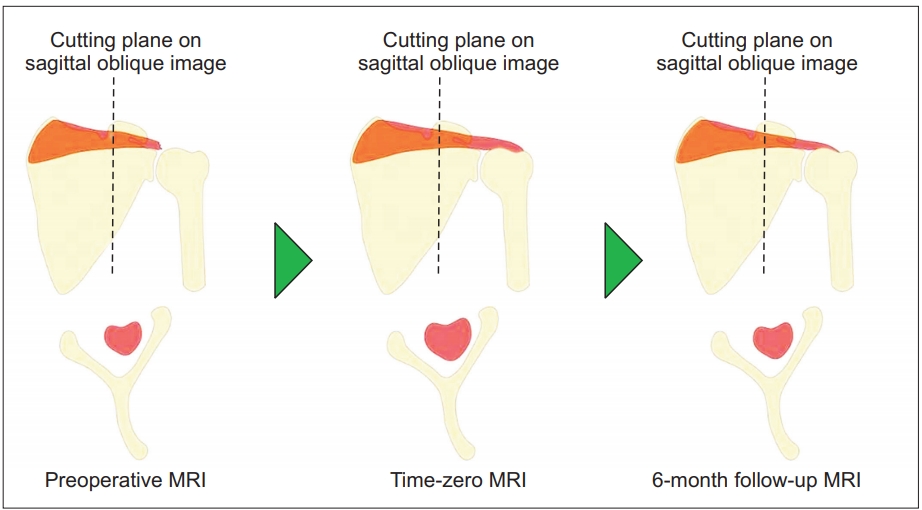
The schematic drawing presents the cross-sectional area of the supraspinatus muscle on the same scapular plane. The cross-sectional area of the supraspinatus was increased immediately after surgery. However, cross-sectional area was decreased without re-tear 1 month after repair. One of the factors that reduced cross-sectional area is thought to be the medial retraction of repaired tendon.
MRI: magnetic resonance imaging.
Our study had the following strengths: (1) a relatively large number of patients who underwent MRI at 3 time points: preoperative, at time-zero, and at 6-month follow-up; (2) all MRIs were performed at a single institution using the same protocol and high resolutions; (3) measurements were performed twice by 2 different investigators who were unaware of the outcomes.
However, our study also has several limitations: (1) as time-zero MRI was taken the day after surgery, the volume measurement might have increased due to saline edema; (2) although we tried to choose the same scapular plane view as much as possible, small differences during MRI were unavoidable due to patient position and cutting sequence of 3 mm, resulting in slight differences in the 3 cut images from the same patient. In addition, 2 measurements were done by different 2 orthopedic surgeons, leading to the probability of measurement bias; (3) the repair method was not standardized, and a mixture of single row and double rows was used, resulting in the occurrence of some technical bias; (4) the study subjects were limited to those who were willing to undergo MRI at 3 time points; thus, not all patients were included consecutively, thereby introducing sampling bias; (5) we did not compare the same number of patients by tear size, which could lead to a bias in the results; (6) an additional 4 years of follow-up MRI would be more desirable to compare and see the long-term effect of the repair.
Conclusion
Immediate changes showing morphologic improvement are observed in the Goutallier stage, Thomazeau grade, and cross-sectional area of the supraspinatus after successful arthroscopic rotator cuff repair, as measured by MRI from time-zero. Furthermore, the muscle cross-sectional area significantly decreased (11.41%) from time-zero to 6 months, but the Goutallier stage and Thomazeau grade did not change significantly. The cross-sectional area of the initial repair appears to decrease a few months postoperatively, which was possibly due to medial retraction or strained muscle.
Notes
Research Ethics
IRB approval: Samsung Medical Center (No. SMC: 2016-02-019).
Conflict of interest
None.
Financial support
None.