|
 |
- Search
| Clin Shoulder Elb > Volume 22(1); 2019 > Article |
|
Abstract
Background
Glenoid baseplate location is important to good clinical outcomes of reverse total shoulder arthroplasty (RTSA). The glenoid vault is the determining factor for glenoid baseplate location, but, to date, there are no reports on the effect of central cage location within the glenoid vault on RTSA outcomes when using the Exactech® Equinoxe® Reverse System. The purpose of this study was to determine the appropriate cage location in relation to the glenoid vault and monitor for vault and/or cortex penetration by the cage.
Methods
Data were retrospectively collected from the Samsung Medical Center (SMC) and Seoul National University Bundang Hospital (SNUBH). Patients who underwent RTSA between November 2016 and February 2018 were enrolled. Glenoid vault depth, central cage location within the vault were examined. Inferior glenoid rim–center distance, inferior glenoid rim–cage distance, and center–cage center distances were collected.
Results
Twenty-two patients were enrolled. Three SNUBH patients had inappropriate central cage fixation (33.3%) versus 4 SMC patients (30.8%). All cage exposures were superior and posterior to the glenoid vault. Mean center–cage distance was 5.0 mm in the SNUBH group and 5.21 mm in the SMC group. Center–prosthesis distance was significantly longer in the inappropriate fixation group than in the appropriate fixation group (p<0.024).
Reverse total shoulder arthroplasty (RTSA) can provide a predictable level of pain relief and functional recovery [1]. While RTSA outcomes may be excellent, patient satisfaction can be improved. Previous clinical studies have emphasized how internal rotation (IR) and external rotation (ER) limitations after RTSA can affect daily living activities [2]. Gutiérrez et al. [3] evaluated the effects of glenoid baseplate positioning on range of motion adduction and abduction of the shoulder after RTSA. Their results indicated that lateralization, inferior translation, inferior tilt, and alteration in the humeral neck–shaft angle were the most important factors for increasing the full arc of abduction and minimizing inferior notching. In cadaveric models, Li et al. [4] found that superior translation of the glenosphere resulted in significant shoulder IR and ER restrictions after RTSA.
Based on the results of these studies, glenoid baseplate location is important to good clinical RTSA outcome. However, glenosphere fixation at the glenoid is also a critical factor in RTSA outcome. For solid fixation of the glenoid component to occur, the baseplate must be placed in the glenoid vault (in place of the cancellous bone) medial to the glenoid articular surface. Penetration of the cortex or improper fixation of the central peg can alter RTSA longevity. Rispoli et al. [5] studied the association between the center point of the glenoid surface and the glenoid vault and concluded that the center point of the glenoid vault is slightly anterior and inferior to the center point projected from the surface. Thus, the operator may misinterpret the location of glenoid vault when positioning the glenoid baseplate.
The glenoid vault is the determining factor for appropriate glenoid baseplate positioning, but there are no reports on the correlation between central cage location in RTSA and the glenoid vault. The aim of this study was to determine an appropriate cage location in relation to the glenoid vault and to monitor RTSA outcomes for subsequent vault or cortex penetration.
We chose to assess a standard RTSA glenoid plate, the Exactech ® Equinoxe® Reverse System (Exactech, Gainesville, FL, USA) (Fig. 1) in this study. The Equinoxe® has an eccentric design suitable for distal shifting into the glenosphere and for inferior overhanging. It has a central cage for bone graft placement, which can promote bony ingrowth. Because of its eccentric design, we hypothesized that the surgeon can achieve inferior flushing easily but may experience difficulty placing the central cage within the glenoid vault.
Data were retrospectively collected from records at the Samsung Medical Center (SMC) and the Seoul National University Bundang Hospital (SNUBH). Patients who underwent RTSA with the Equinoxe® Reverse System (Fig. 1) between November 2016 and February 2018 were enrolled. All operations were performed by two highly skilled surgeons at each center. All patients underwent a preoperative computed tomography (CT) shoulder scan and a postoperative CT shoulder scan at 3 to 6 months follow-up visit. From the preoperative scan, glenoid vault depth was determined (Fig. 2). Maximal glenoid vault depth was evaluated on axial, coronal, and sagittal CT images of the glenoid. Location and appropriate fixation in the vault of central cage were evaluated on the postoperative CT scan. The inferior glenoid rim–center, inferior glenoid rim–cage, and center–cage center distances were determined postoperatively to assess the association the central cage and the vault (Fig. 3). For evaluation of central cage location, the patient outcomes were divided into three groups: group A, cage out of the vault, superior position (Fig. 4); group B, cage in the vault, but superior position (Fig. 5); and group C, cage in the vault, appropriate position (Fig. 6). Statistical analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC, USA). A p-value of <0.05 was considered statistically significant.
A total of 22 patients (5 males, 17 females) were enrolled in the study: 9 from SNUBH and 13 from SMC. On the preoperative CT scans, mean glenoid vault depth in the male was 30.34 mm, while that in the female was 24.26 mm. On the postoperative CT scan, 3 patients from SNUBH had inappropriate central cage fixation (33.3%) and 4 patients from SMC had inappropriate central cage fixation (30.8%) (Table 1) and all exhibited penetration of the cortex. All cases of central cage exposure from the vault were superior to and posterior in the glenoid vault. Mean center–cage distance was 5.0 mm in the SNUBH patients and 5.21 mm in the SMC patients (Table 2). The center–prosthesis distance was significantly longer in the inappropriate fixation group than in the appropriate fixation group (p<0.024).
Previous studies have examined the anatomical shoulder characteristics of Asian populations treated with RTSA, especially in subjects with small glenoid and humeral head sizes. Ji et al. [6] compared the component sizes of RTSA devices, especially the glenoid component, to the glenoid bony size in a Korean population. In their anatomical study, mean radius of the anatomic inferior cortical rim of the glenoid was 15.4 ± 1.6 mm in Korean females and 17.1 ± 2.1 mm in Korean males. The authors reported that it was difficult to insert a 29 mm diameter glenoid baseplate and reamer to the smaller glenoid in the Korean population because the lengths and diameters of the humeral diaphysis of Asians, especially females, were smaller than those of Caucasians. They also observed that firm screw fixation of compression screws in the metaglene was possible in only 59.5% (25/42 cases) of their subjects. This might be due to the relatively small anterior or posterior glenoid bone stock, which can result in less rigid fixation. Thus, they concluded that the use of a more appropriately sized glenoid RTSA component should be considered.
Similarly, Matsumura et al. [7] described the glenohumeral geometry of a normal Japanese study population. The anthropometric analysis of the glenohumeral joint was performed using CT scans of 160 normal shoulders from healthy Japanese volunteers. They reported that the Japanese glenoid height was 12% shorter than that in male non-Asian shoulders and 16% shorter than that in female non-Asian shoulders. Moreover, the glenoid width was 16% narrower than that in male non-Asian shoulders and 21% narrower than that in female non-Asian shoulders. Their results can be useful in determining implant sizes and in improving shoulder prosthesis design to reflect the normal anatomy of the Asian glenohumeral joint. They also recommend that if the contralateral shoulder remains intact, then its parameter values should be applied for the shoulder undergoing RTSA.
In the present study, we detected no difference in cage penetration of the cortex or improper positioning within vaults between male and female patients. However, the mean glenoid vault size of the male patients was 30.34 mm, while that of the female patients was 24.26 mm on preoperative CT scans. Because of our small number of male cases, additional male patients should be examined in order to evaluate the possible significance of sex-based differences in glenoid vault depth.
We hypothesized that placing the glenoid baseplate’s central cage within the glenoid vault is difficult because of its eccentric design. In our study, central cage glenoid cortical perforation occurred in 3 cases (33.3%) at SNUBH and 4 cases (30.8%) at SMC. Simovitch et al. [8] estimated that a larger peg–glenoid rim distance, reflecting higher positioning of the metaglene and thus the glenosphere, was correlated with an increased frequency of inferior notching. In the present study, we estimated inferior glenoid rim–center, inferior glenoid rim–cage, and center–cage center distances. The center–prosthesis distance was significantly longer in the inappropriate fixation group than in the appropriate fixation group (p<0.024). Because Asian populations have a smaller superior-inferior glenoid diameter than that of Caucasians, it is important for the surgeon to carefully determine the position of the central cage within the vault.
We recommend that, during standard baseplate placement in a small glenoid, the cage be positioned lower than usually targeted, and allow it to overhang the inferior rim. During the placement of small baseplates, a slight overhang should be used, as well as horizontal placement of an inferior screw or the use of a slightly larger sphere in order to maintain a 2 to 4 mm overhang.
The Equinoxe® RTSA device gained clearance in Korea in 2015 and in Japan in 2017. Subsequently, feedback, similar to that in our study has been gathered for the device’s smaller glenoid baseplates. Exactech® reviewed the information and subsequently developed a small glenoid plate that is optimized for the Asian glenohumeral anatomy. The new smaller baseplate should possess a smaller glenosphere size to allow easy application in total shoulder arthroplasty to conversional RTSA by using the same center screw, as well as allowing for optimized component overhanging.
There are some limitations to this study. First, it was retrospective and included a small number of patients, particularly male patients. Second, it was not randomized and its follow-up duration was short. However, by optimizing the available preand postoperative CT scans, we were able to simultaneously calculate vault depth and central cage location. Despite the small number of cases, this study’s findings support the use of a smaller baseplate during RTSA of the relatively small glenoid structure of Asian patients.
In conclusion, in most patients in this study, the central cage was to be placed in a superoposterior direction in the vault. Thus, the surgeon needed to be cautious about the location of the central cage in relation to the glenoid vault. Thus, the surgeon needed to be cautious about the location of the central cage in relation to the glenoid vault. To ensure appropriate fixation of the glenoid baseplate in the glenoid vault, especially in patients with small glenoids, we, therefore, recommend that cage placement be lower than usually targeted, and it should overhang the inferior glenoid rim.
NOTES
Fig. 1.
Illustration of glenoid baseplate (Equinoxe® Reverse system; Exactech®, Gainesville, FL, USA) (permission from Exactech).
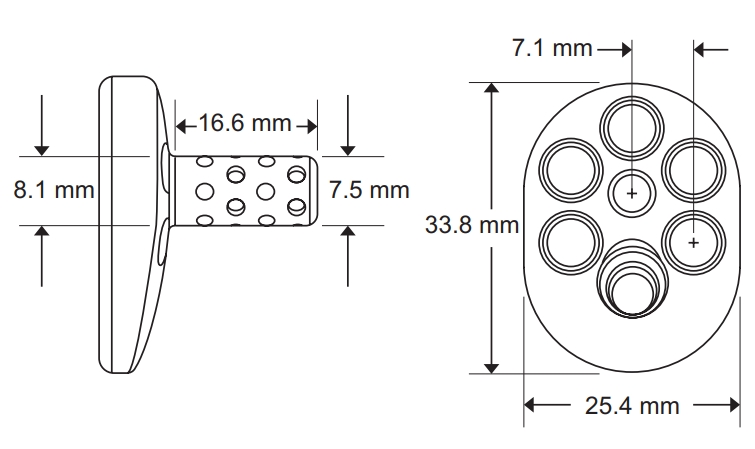
Fig. 3.
Estimation of central cage center (permission from Exactech).
A: inferior glenoid rim–center distance, B: inferior glenoid rim–cage distance, C: center–cage center distance=‘A’+3.75 mm (half radius of central peg)-‘B’.
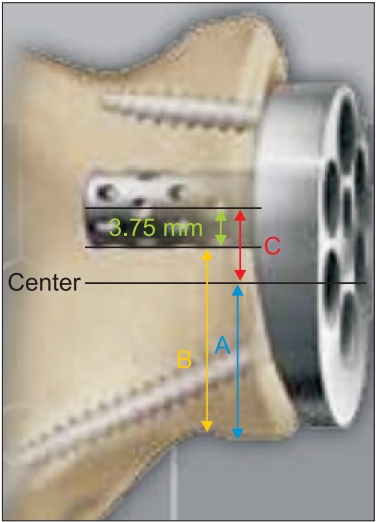
Fig. 4.
Group A. Out of the vault, superior position. (A) Preoperative X-ray and computed tomography (CT) scan. (B) Postoperative X-ray and CT scan.
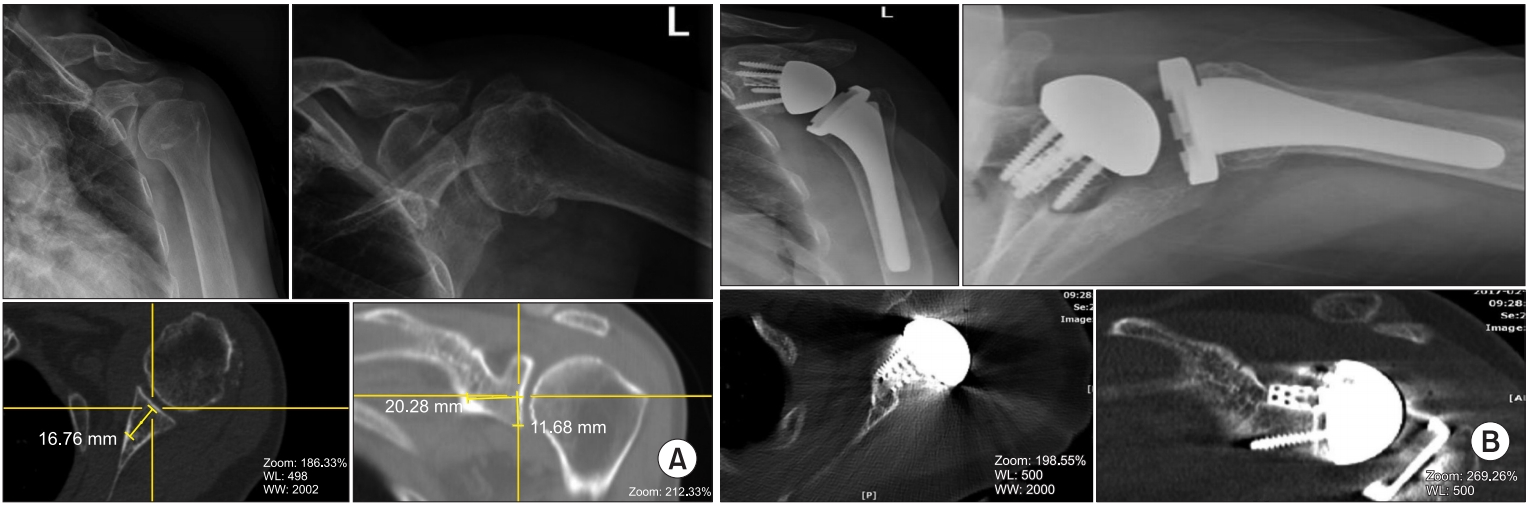
Fig. 5.
Group B. In the vault, superior position. (A) Preoperative X-ray and computed tomography (CT) scan. (B) Postoperative X-ray and CT scan.
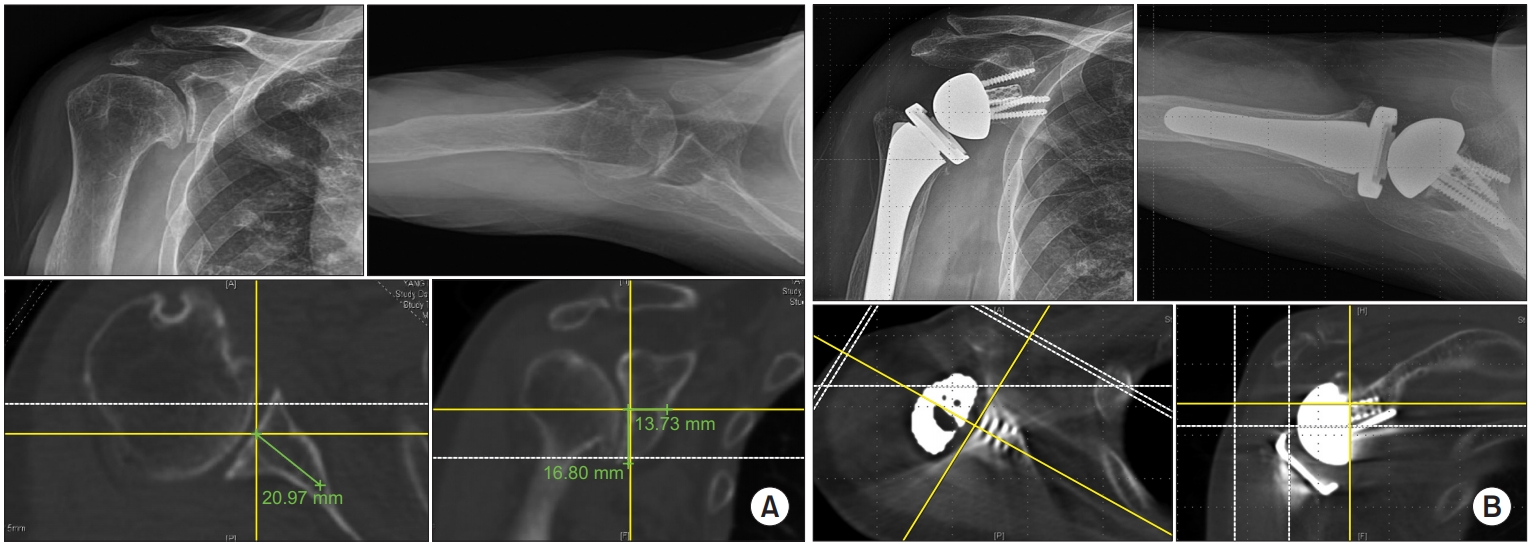
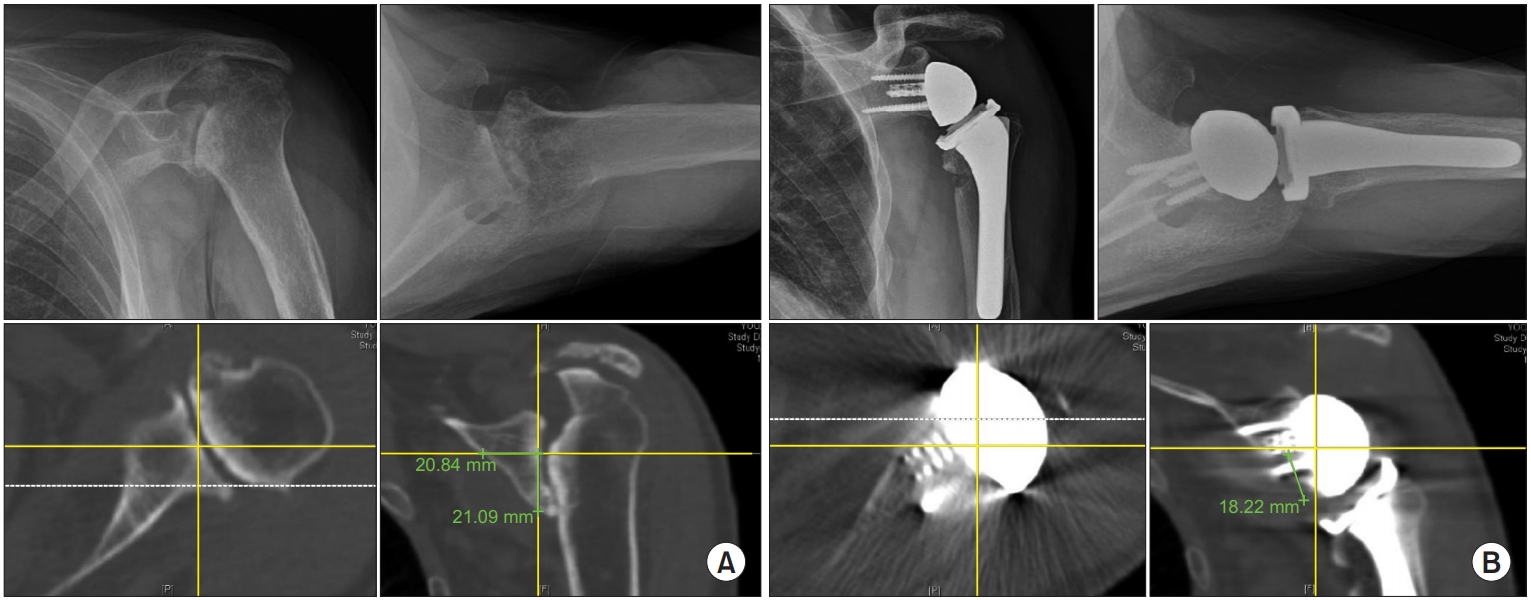
Fig. 6.
Group C. In the vault, appropriate position. (A) Preoperative X-ray and computed tomography (CT) scan. (B) Postoperative X-ray and CT scan.
References
1. Boileau P, Gonzalez JF, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009;18(4):600–6. doi: 10.1016/j.jse.2009.03.011.


2. Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005;87(7):1476–86.


3. Gutiérrez S, Levy JC, Frankle MA, et al. Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg 2008;17(4):608–15. doi: 10.1016/j.jse.2007.11.010.


4. Li X, Knutson Z, Choi D, et al. Effects of glenosphere positioning on impingement-free internal and external rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2013;22(6):807–13. doi: 10.1016/j.jse.2012.07.013.


5. Rispoli DM, Sperling JW, Athwal GS, Wenger DE, Cofield RH. Projection of the glenoid center point within the glenoid vault. Clin Orthop Relat Res 2008;466(3):573–8. doi: 10.1007/s11999-007-0087-1.



6. Ji JH, Jeong JY, Song HS, et al. Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg 2013;22(8):1102–7. doi: 10.1016/j.jse.2012.07.019.


- TOOLS
-
METRICS

-
- 4 Crossref
- 25,941 View
- 264 Download
- Related articles in Clin Should Elbow